G6PD Deficiency Risk Assessment Tool
This tool helps determine your risk of drug-induced hemolytic anemia if you have G6PD deficiency. G6PD deficiency affects up to 14% of African American men and 4-15% of people of Mediterranean descent. Certain medications can trigger severe red blood cell destruction in these individuals.
Risk Assessment Form
When a medicine you take starts attacking your own red blood cells, it’s not just a side effect-it’s a medical emergency. Drug-induced immune hemolytic anemia (DIIHA) happens when your immune system, confused by a drug, turns against your red blood cells and destroys them. These cells normally live for about 120 days. In DIIHA, they’re shredded in days-or even hours. The result? Severe fatigue, yellowing skin, rapid heartbeat, and in worst cases, heart failure. It’s rare, but when it happens, missing the signs can be deadly.
How Medications Trigger Red Blood Cell Destruction
Not all drug-induced hemolysis works the same way. There are two main paths: immune-mediated and oxidative.
In immune-mediated DIIHA, the drug sticks to your red blood cells like a hidden tag. Your body sees this new combo as an invader and makes antibodies to destroy it. The most common culprits? Cephalosporins, especially cefotetan, ceftriaxone, and piperacillin. Together, these antibiotics cause about 70% of all immune-mediated cases. Other offenders include penicillin, methyldopa, and levodopa. The catch? Symptoms don’t show up right away. You usually need 7 to 10 days of continuous use before your immune system flips the switch.
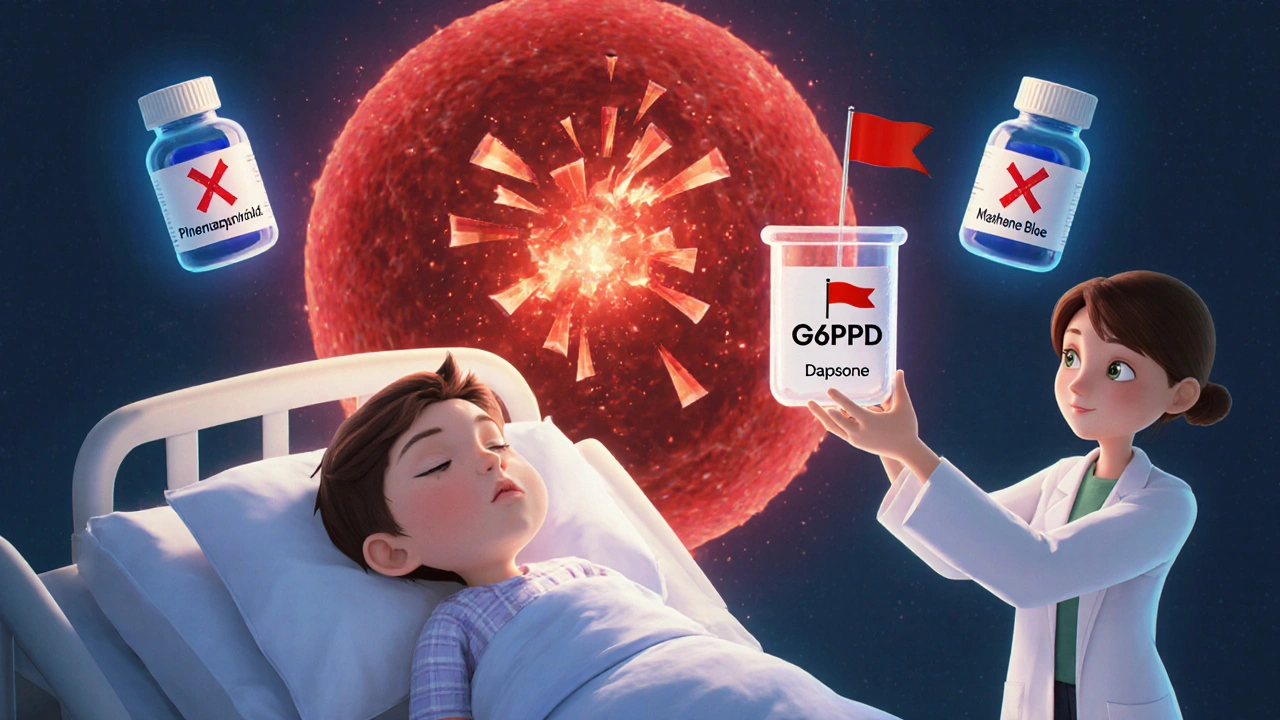
Oxidative hemolysis is different. It doesn’t involve antibodies. Instead, certain drugs create a chemical storm inside red blood cells, damaging hemoglobin. This leads to clumps called Heinz bodies, which make cells fragile and prone to bursting. This type hits fast-sometimes within 24 to 72 hours. The biggest risk factor? G6PD deficiency. This genetic condition affects up to 14% of African American men and 4-15% of people of Mediterranean descent. Even if you’ve never had a problem before, a single dose of dapsone, phenazopyridine (Pyridium), primaquine, or nitrofurantoin can trigger a crisis. And here’s the twist: methylene blue, often used to treat severe methemoglobinemia, can make this worse. It’s absolutely dangerous for people with G6PD deficiency.
What Symptoms Should You Watch For?
The early signs are easy to miss. They look like the flu, a bad cold, or just general exhaustion. But if you’re on a new medication and start feeling off, don’t brush it off.
- Fatigue-reported in 92% of cases
- Weakness-87% of patients
- Shortness of breath-even with light activity
- Rapid heartbeat-over 100 beats per minute
- Pale skin-especially in the face, palms, or eyelids
- Jaundice-yellowing of the skin or whites of the eyes
These symptoms don’t appear gradually. In acute cases, hemoglobin can drop 3 to 5 grams per deciliter in just 48 to 72 hours. That’s like losing a full liter of blood overnight. People with very low hemoglobin-below 6 g/dL-face real risks: arrhythmias, cardiomyopathy, even heart failure. Children are especially vulnerable. Studies show pediatric cases often present with hemoglobin levels as low as 5.2 g/dL, much lower than adults’ average of 6.8 g/dL.
How Doctors Diagnose It
There’s no single test. Diagnosis is a puzzle made of symptoms, history, and lab results.
First, doctors look for signs of hemolysis:
- Elevated indirect bilirubin-above 3 mg/dL
- High LDH-above 250 U/L
- Low haptoglobin-below 25 mg/dL
These three markers together strongly suggest red blood cells are being destroyed. Next, a blood smear under the microscope reveals the type:
- Spherocytes-small, round, dense red cells-point to immune-mediated DIIHA
- Heinz bodies-dark clumps inside red cells-signal oxidative damage
The gold standard for immune-mediated cases is the direct antiglobulin test (DAT). It detects antibodies stuck to red blood cells. It’s positive in 95% of immune-mediated DIIHA cases. But here’s the catch: it can be negative early on, or if the drug causes a rare type of antibody that doesn’t bind well. That’s why doctors can’t rely on it alone.
If G6PD deficiency is suspected, testing is tricky. During active hemolysis, the test can give a false negative. Why? The assay measures enzyme levels in older red blood cells-the ones already destroyed. The new cells (reticulocytes) still have normal G6PD. So, testing should wait 2 to 3 months after the episode. If you’ve had a sudden hemolytic reaction after taking a drug like dapsone or phenazopyridine, assume G6PD deficiency until proven otherwise.

What Happens When You Stop the Drug?
The most important step? Stop the medicine. Immediately.
In over 95% of cases, hemolysis slows down within 7 to 10 days after removing the trigger. Most people fully recover in 4 to 6 weeks. But stopping the drug isn’t always enough.
If hemoglobin drops below 7-8 g/dL, or if symptoms are severe-dizziness, chest pain, trouble breathing-a blood transfusion may be needed. But transfusions carry risks in DIIHA. The immune system may attack the new cells too. So doctors choose carefully, matching blood types and sometimes using washed red cells.
For immune-mediated cases that don’t improve, corticosteroids like prednisone (1 mg/kg/day) are often tried. But evidence is weak. Many patients improve without them. If the anemia persists beyond a few weeks, it may mean the body has started making its own antibodies-now independent of the drug. That’s when stronger drugs kick in: intravenous immunoglobulins (1 g/kg/day for two days), then rituximab (375 mg/m² weekly for four weeks), or azathioprine or cyclosporine. About 78% of these refractory cases respond within 3 to 6 weeks.
For oxidative hemolysis with severe methemoglobinemia (over 30%), methylene blue is life-saving-but only if G6PD is normal. Give it to someone with G6PD deficiency, and you’ll make the hemolysis worse. Always check before administering.
Hidden Dangers and Common Mistakes
Doctors miss DIIHA more often than you’d think. One 2024 study found 43% of cases were initially misdiagnosed as infections, autoimmune diseases, or other types of anemia.
Another trap? Assuming a drug is safe because you’ve taken it before. DIIHA can develop after months or years of use. Methyldopa, once common for high blood pressure, caused hemolysis in many patients over time-even those who’d taken it for years without issue.
And here’s something many don’t realize: DIIHA can make your blood hypercoagulable. A 2023 study showed 34% of severe cases developed blood clots-deep vein thrombosis or pulmonary embolism. So even if you’re anemic, you might still need blood thinners. That’s counterintuitive, but critical.
Children are often overlooked. Their symptoms are more dramatic, but doctors may assume it’s something else. Pediatric cases are rare-but when they happen, they’re serious.
What’s New in Diagnosis and Prevention
Technology is helping. Hospitals that added alerts in their electronic health records for high-risk drugs like ceftriaxone or dapsone saw a 32% drop in severe DIIHA cases over 18 months. These alerts remind clinicians to check for hemolysis markers before prescribing.
Research is also moving forward. Two clinical trials in 2024 showed promise:
- NCT05678901 tested efgartigimod, a drug that clears antibodies. It worked in 67% of patients within four weeks.
- NCT05812345 is studying complement inhibitors to block the immune system’s attack on red cells.
The International Society of Hematology is also working on updated diagnostic criteria to better distinguish drug-dependent antibodies from drug-independent ones. This could change how we test and treat.
What You Can Do
If you’re on any medication and suddenly feel unusually tired, pale, or short of breath-especially after starting a new drug-tell your doctor. Mention the timing. Did the symptoms start after 7-10 days? That’s a red flag for immune-mediated DIIHA. Did they hit within 48 hours? Think oxidative.
Keep a list of all your medications-including over-the-counter and herbal supplements. Some herbal products can trigger hemolysis too.
If you’re of African or Mediterranean descent, ask your doctor about G6PD testing-even if you’ve never had a problem. It’s a simple blood test. Knowing your status could save your life when you need antibiotics or pain relief.
And if you’ve ever had unexplained anemia after taking a drug, don’t ignore it. Even if you recovered, the risk is still there. Avoid that drug forever. Write it down. Tell every new doctor.
Drug-induced hemolytic anemia is rare. But when it strikes, speed saves lives. Recognizing it early isn’t just about lab values-it’s about listening to your body and asking the right questions.
Can any medication cause hemolytic anemia?
Yes, but not all. Over 100 drugs are linked to hemolytic anemia, mostly antibiotics like cephalosporins, pain relievers like NSAIDs, and certain antimalarials. The most common are cefotetan, ceftriaxone, piperacillin, dapsone, and phenazopyridine. Even drugs you’ve taken safely before can trigger it later.
How long does it take for symptoms to appear after taking a drug?
It depends on the mechanism. Immune-mediated DIIHA usually takes 7 to 10 days of continuous use. Oxidative hemolysis can happen within 24 to 72 hours, especially in people with G6PD deficiency. If you’ve taken the drug before without issues, symptoms can still appear after months or years.
Is hemolytic anemia from drugs dangerous?
It can be. While mild cases resolve after stopping the drug, severe cases can cause rapid drops in hemoglobin, leading to heart failure, arrhythmias, or blood clots. In children, it’s often more severe. Prompt diagnosis and stopping the drug are critical to survival.
Can I get tested for G6PD deficiency before taking risky medications?
Yes, and it’s recommended if you’re of African, Mediterranean, or Southeast Asian descent. Testing is simple and done with a blood sample. If you’re deficient, you’ll need to avoid over 100 medications that can trigger hemolysis-including common painkillers and antibiotics. Knowing your status prevents crises.
Why is methylene blue dangerous in some cases?
Methylene blue is used to treat severe methemoglobinemia, a condition where hemoglobin can’t carry oxygen properly. But in people with G6PD deficiency, methylene blue itself causes oxidative stress that destroys red blood cells. It can trigger a life-threatening hemolytic crisis. Always confirm G6PD status before giving it.
Will I always have this problem if I’ve had drug-induced hemolytic anemia once?
You won’t have ongoing anemia after recovery-but you’ll always be at risk if you take the same drug again. Once your immune system has reacted to a drug, it remembers it. Re-exposure can cause a faster, more severe reaction. Avoid the triggering medication for life. Tell every healthcare provider you see.



13 Comments
Timothy Reed
Great breakdown of DIIHA-this is exactly the kind of info that should be in every primary care provider’s quick-reference guide. The distinction between immune-mediated and oxidative is critical, and the timing notes (7–10 days vs. 24–72 hours) are gold. I’ve seen this misdiagnosed as ‘viral fatigue’ too many times. Thanks for highlighting the G6PD trap with methylene blue-that’s a silent killer in ERs.
Christopher K
Of course it’s rare-because Big Pharma doesn’t want you to know how many of their drugs are basically poison. Ceftriaxone? That’s a 1000mg hammer to your immune system. They make billions selling it, then charge you extra to fix the mess they made. Wake up people.
harenee hanapi
OMG I knew this was happening to me last year when I took phenazopyridine for my UTI-I turned yellow and felt like I was dying but my doctor just said ‘it’s stress’ 😭 I’m so glad someone finally said it out loud. I’m telling everyone. This is a cover-up. I cried reading this. I feel seen.
Christopher Robinson
So much good info here 🙌 I’ve had patients with G6PD deficiency get hit by nitrofurantoin and think it’s ‘just a bad reaction’-this is why we need screening before prescribing. Also, the clotting risk? Mind blown. Never thought anemia could make you hypercoagulable. Adding this to my med ed deck. 🧠❤️
Brian Rono
Let’s be honest: this isn’t ‘rare.’ It’s underreported because clinicians are lazy. You don’t check haptoglobin? You don’t look at smears? You just order a CBC and call it ‘iron deficiency’? That’s malpractice dressed in white coats. The DAT being negative doesn’t mean it’s not DIIHA-it means you didn’t look hard enough. And yes, methyldopa? Still on the market? In 2024? Unbelievable.
Zac Gray
I appreciate the depth here, but let’s not pretend this is new. I’ve been warning my residents about ceftriaxone and hemolysis since 2018. The fact that this is still a diagnostic blind spot says more about our training system than the disease itself. And yes-methylene blue in G6PD deficiency? That’s not just dangerous. It’s criminal. We have protocols. We just don’t follow them. I’m not mad. I’m just… tired.
Steve and Charlie Maidment
So you’re saying if I took ceftriaxone once and got tired, I should never take it again? What if I have a life-threatening infection? Am I supposed to die because some guy on Reddit wrote a 10-page essay? And why are we even talking about this? It’s not like people are lining up to get hemolytic anemia. This feels like fearmongering wrapped in a lab coat.
Michael Petesch
Fascinating. In India, we see G6PD deficiency more frequently than most Western clinics acknowledge. I’ve had young men come in after taking dapsone for leprosy-no prior history, no symptoms, then sudden hemolysis. The cultural stigma around ‘blood disorders’ often prevents testing. This post should be translated and circulated in rural clinics. Knowledge is the first vaccine.
Ellen Calnan
There’s something spiritual about the body screaming back when you force it to accept something foreign. This isn’t just medicine-it’s a conversation between biology and chemistry. And when the body says ‘no,’ we don’t listen. We prescribe more. We ignore the fatigue. We call it ‘anxiety.’ But the red blood cells-they don’t lie. They shatter. And when they do, they’re begging you to pay attention. Maybe the real illness isn’t the drug. It’s our arrogance.
Richard Risemberg
Man, this is the kind of post that makes me proud to be in healthcare. You didn’t just list drugs-you explained the *why*. The Heinz bodies, the DAT pitfalls, the G6PD testing timing… this is textbook material, but written like a human. I’m printing this for my med students tomorrow. Also-methylene blue = enemy #1 in G6PD? Yeah. That’s the kind of pearl you only learn after someone almost dies.
Andrew Montandon
Wow. Just… wow. I’ve been on ceftriaxone twice-once for pneumonia, once for a dental abscess. Both times I felt weirdly exhausted for a week after. I thought it was just ‘the antibiotics.’ Now I’m scared. I’m going to my doctor tomorrow to get my G6PD tested. And I’m writing ‘CEFTORIAXONE - DO NOT USE’ on my medical alert bracelet. Thank you for this. Seriously. This could save my life.
Sam Reicks
they want you to think its the drugs but its the vaccines that are destroying your rbc's and the gmo foods and the fluoride in the water and the 5g towers. they dont want you to know. i had hemolytic anemia after my flu shot. they gave me blood and it turned black. the hospital is lying. they're all in on it. you think ceftriaxone is bad? wait till you see what's in the vaccines. i saw it on a forum. it's real. trust me. i'm not crazy. the system is.
seamus moginie
Well done. A textbook case of clinical excellence. The distinction between immune and oxidative pathways is precise, the drug list comprehensive, and the diagnostic red flags crystal clear. That 34% clotting statistic? Chilling. And the fact that children present with hemoglobin as low as 5.2 g/dL? That’s not just rare-it’s terrifying. This should be mandatory reading for every intern. I’ve shared it with my entire department. Thank you for writing this with such clarity and gravity.