Lupus Check-Up Frequency Calculator
Lupus Check-Up Frequency Calculator
Enter your lupus type and current condition to determine the recommended frequency for your medical check-ups.
Recommended Check-Up Frequency
Living with lupus means keeping an eye on a disease that can flare up in the skin, joints, kidneys, or even the heart. Whether you have Discoid Lupus Erythematosus, a skin‑limited form, or Systemic Lupus Erythematosus, a whole‑body condition, regular medical visits are the single most effective way to catch problems early and adjust treatment before symptoms become severe.
Key Takeaways
- Check‑ups every 3-6 months are a proven way to reduce organ damage.
- Blood tests (ANA, anti‑dsDNA, CBC) and urine analysis reveal hidden inflammation.
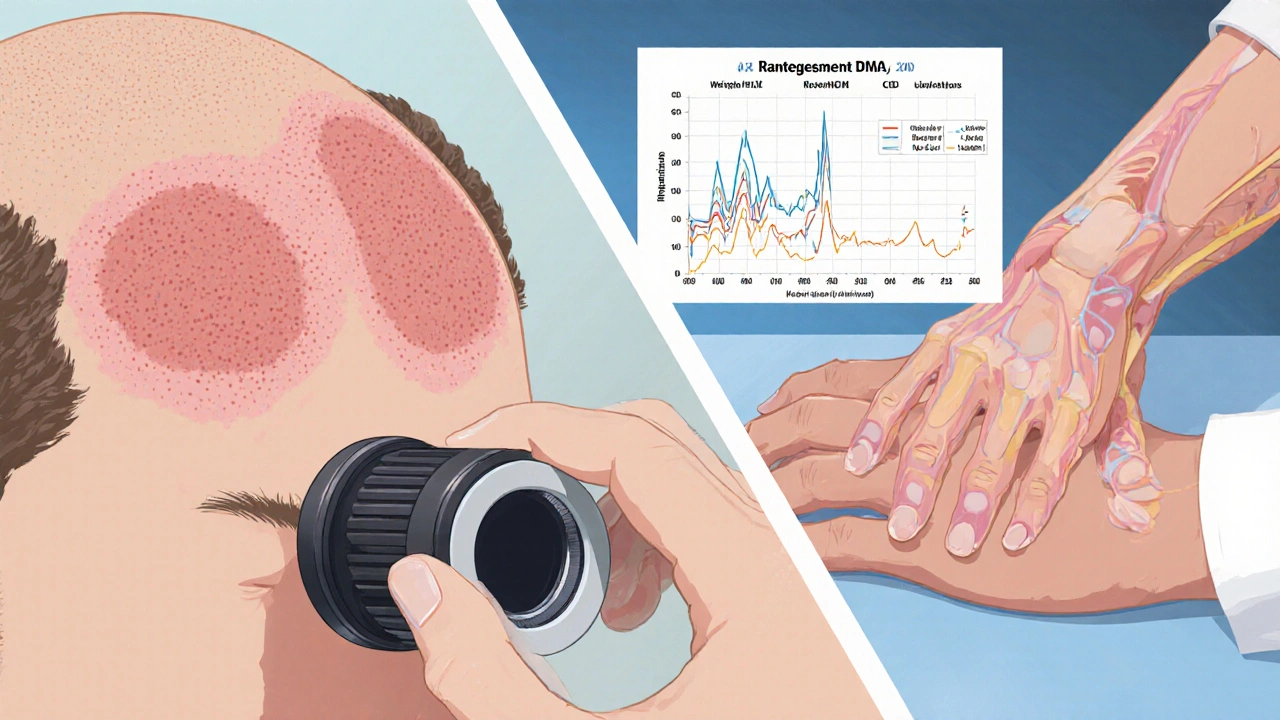
- Dermatologists monitor skin lesions for DLE, while rheumatologists track internal organ involvement for SLE.
- Knowing the red‑flag symptoms-new joint pain, swelling, fever, or a sudden rash-lets you seek urgent care.
- A simple patient checklist can keep appointments, labs, and medication refills on track.
Understanding Discoid and Systemic Lupus
Discoid Lupus Erythematosus is a chronic, skin‑focused form of lupus that causes round, scarring plaques, often on the face, scalp, or ears. The lesions can be painful and may lead to permanent hair loss, but they usually do not affect internal organs.
Systemic Lupus Erythematosus, in contrast, is an autoimmune disease that can involve the kidneys, heart, lungs, brain, and blood cells. About 30% of people with DLE eventually develop SLE, so regular monitoring bridges the gap between skin‑only and systemic disease.
Why regular lupus check-ups Are Critical
Research from the Lupus Foundation of America (2024) shows patients who attend semi‑annual visits have a 40% lower risk of developing lupus nephritis compared with those who skip appointments. Early detection of kidney inflammation, for example, allows doctors to start low‑dose steroids or mycophenolate before irreversible scarring occurs.
Beyond organ protection, routine visits improve medication adherence. Hydroxychloroquine, the cornerstone drug for both DLE and SLE, requires yearly eye exams because of rare retinal toxicity. Missing that exam can lead to permanent vision loss.
Psychologically, knowing you have a scheduled review reduces anxiety. Many patients report feeling more in control when they see the same rheumatologist or dermatologist every few months.
Core Components of a Lupus Check‑Up
A comprehensive lupus visit typically includes:
- ANA test - screens for antinuclear antibodies; a rising titer can signal a flare.
- Anti‑dsDNA - highly specific for SLE kidney involvement.
- Complete Blood Count (CBC) - watches for anemia, leukopenia, or thrombocytopenia.
- Urinalysis - looks for protein or blood that indicate nephritis.
- Blood pressure and lipid panel - lupus patients face higher cardiovascular risk.
- Skin examination (for DLE) - dermatologist checks lesion size, scarring, and need for topical steroids.
- Joint assessment - rheumatologist grades swelling, range of motion, and pain.
Some clinics also add a cardiopulmonary ultrasound if shortness of breath or chest pain is present.
Timing and Frequency Guidelines
While individual schedules vary, the following framework works for most patients:
- Stable disease - every 4-6 months.
- Recent flare or medication change - every 1-3 months until stable.
- Pregnancy planning - monthly visits with a maternal‑fetal medicine specialist.
- Kidney involvement - every 6 weeks during active nephritis, then gradually lengthen.
Never wait more than a year without a baseline labs review, even if you feel fine.
The Lupus Care Team
Effective monitoring hinges on teamwork:
- Rheumatologist - leads systemic disease management.
- Dermatologist - handles DLE lesions, sun‑avoidance counseling, and skin‑directed therapies.
- Primary care physician - coordinates vaccinations, depression screening, and general health.
- Nephrologist - consulted when urinalysis shows proteinuria >0.5g/day.
- Ophthalmologist - performs yearly retinal exams for patients on hydroxychloroquine.
Having a single electronic health record that all providers can access reduces duplicate labs and missed alerts.
Red Flags That Require Immediate Attention
If you notice any of these, call your rheumatologist or go to the emergency department:
- Sudden swelling of the legs, face, or hands.
- New onset of dark, thick urine (possible kidney bleed).
- High fever (>38.5°C) without infection signs.
- Painful chest pressure or shortness of breath.
- Severe, non‑healing skin ulcer on a DLE lesion.
Practical Patient Checklist
- Mark next appointment date in phone and on a wall calendar.
- Order labs 1-2 weeks before the visit; bring results to the doctor.
- Pack a medication list (dose, frequency, side effects).
- Record any new symptoms in a symptom diary - date, severity, triggers.
- Check sunscreen (SPF30+), wide‑brim hat, and protective clothing before leaving home.
Comparison: Check‑Up Focus for DLE vs. SLE
| Aspect | Discoid Lupus Erythematosus (DLE) | Systemic Lupus Erythematosus (SLE) |
|---|---|---|
| Primary Specialist | Dermatologist | Rheumatologist |
| Core Labs | ANA, CBC, basic metabolic panel | ANA, Anti‑dsDNA, CBC, Urinalysis, complement levels (C3, C4) |
| Organ Surveillance | Skin lesion mapping, phototherapy response | Kidney function, cardiovascular risk, neuro‑cognitive screening |
| Visit Frequency (stable) | Every 4-6 months | Every 3-4 months |
| Medication Monitoring | Topical steroids, antimalarials (hydroxychloroquine) | Hydroxychloroquine, corticosteroids, immunosuppressants (mycophenolate, azathioprine) |
Frequently Asked Questions
How often should I get blood work if my lupus is well‑controlled?
For stable disease, most specialists order a full panel (ANA, CBC, metabolic panel, complement) every 4-6 months. If you’re on immunosuppressants, the interval may shorten to every 3 months.
Can discoid lupus turn into systemic lupus?
Yes, about 20‑30% of people with DLE develop systemic features over time. Regular check‑ups help catch early organ involvement before it progresses.
Is it safe to stop hydroxychloroquine during pregnancy?
Actually, hydroxychloroquine is considered one of the safest lupus drugs during pregnancy and can reduce flare rates. Never stop without discussing it with your rheumatologist.
What sunscreen is best for lupus‑related photosensitivity?
Look for broad‑spectrum SPF30 or higher, mineral‑based (zinc oxide or titanium dioxide) formulas. Reapply every two hours and after swimming.
When should I see a dermatologist versus a rheumatologist?
If your main issue is a skin rash or plaque, start with a dermatologist. If you have joint pain, fatigue, kidney changes, or abnormal labs, a rheumatologist should lead the care.
Next Steps
1. Review your last lab report; note any values that are out of range.
2. Call your clinic to schedule the next appointment based on the frequency guide above.
3. Update your medication list and bring it to the visit.
4. Start a symptom diary today - even a few lines a day can reveal patterns.
Sticking to a consistent check‑up routine doesn’t cure lupus, but it gives you the best chance to stay ahead of the disease, keep organ damage low, and maintain quality of life.


10 Comments
Winnie Chan
Congrats on the ultimate lupus checklist, now I can finally pretend I’m organized. It's like having a cheat sheet for a disease that loves surprises.
Kyle Rensmeyer
They don't want you to see the real reason for those check‑ups 🤔 pharma push, hidden agendas everywhere.
Rod Maine
Honestly this article reads like a 10‑page PowerPoint from a med school lecture-so academic but still somehow reely boring. I mean, who needs that much jargon when a simple list would do?
Othilie Kaestner
Sure, the CDC says quarterly labs are fine, but in America we should be seeing a doc every month - no excuses. If we can launch rockets, we can schedule more check‑ups.
Sebastian Samuel
💥🔬 Regular labs are the frontline defense, and you can't skimp on that. I keep my calendar full, and I make sure to flag any new meds ☝️.
Mitchell Awisus
I totally agree that keeping a regular Lupus check‑up schedule is a game‑changer for patients; first, consistent lab work catches subtle shifts in ANA titers before a full‑blown flare. Second, the kidney function tests are absolutely essential because early nephritis can be silent; third, the eye exams for hydroxychloroquine toxicity are non‑negotiable, eyesight is priceless. Fourth, having a symptom diary empowers patients to communicate patterns to their rheumatologist, and fifth, aligning appointments with both a dermatologist and rheumatologist reduces duplicated tests. Sixth, the multidisciplinary approach also allows the primary care doctor to monitor cardiovascular risk, which is often overlooked. Seventh, scheduling visits every 4‑6 months for stable disease aligns with the evidence from the Lupus Foundation; eighth, if a flare occurs, tightening the interval to 1‑3 months provides rapid response. Ninth, pregnancy planning should involve monthly visits with a maternal‑fetal specialist to safeguard both mother and baby; tenth, the extra monitoring after medication changes catches side‑effects early, which can prevent irreversible damage. Eleventh, many patients report lower anxiety levels when they have a concrete calendar of appointments, and twelfth, this sense of control often translates into better medication adherence. Thirteenth, let’s not forget the role of lifestyle counseling - sun protection, diet, and exercise are all discussed during visits; finally, the cumulative effect of these strategies is a higher quality of life and fewer hospitalizations.
Annette Smith
Regular check‑ups give you a clear picture of what’s happening inside. When you track labs and symptoms, you can act before things get bad.
beth shell
Check‑ups are the backbone of lupus care. They keep the disease in check.
khushali kothari
From a clinical informatics perspective, the integration of longitudinal biomarker trajectories (e.g., anti‑dsDNA fluctuations) with patient‑reported outcome measures facilitates early detection of subclinical activity. Moreover, the implementation of an interoperable EHR module that auto‑generates reminder alerts mitigates missed appointments. The evidence base underscores a statistically significant reduction in progression to lupus nephritis when follow‑up intervals are ≤ 4 months for high‑risk cohorts. Consequently, adherence to a structured schedule is not merely a recommendation but a quantifiable risk‑mitigation strategy. Finally, patient empowerment through digital symptom diaries synergizes with provider surveillance, optimizing therapeutic windows.
Brandon Smith
We have a moral obligation to hold the healthcare system accountable for ensuring these check‑ups are accessible to every lupus patient. Anything less is an ethical failure. The data clearly show improved outcomes with regular monitoring, yet many are denied because of cost barriers. This disparity must be addressed now.