Blood Pressure Medication Safety Checker
Safety Assessment Tool
This tool helps you determine if CoQ10 supplementation is likely safe with your current blood pressure medications. Based on information from medical studies and expert guidelines.
When you're managing high blood pressure, every pill, every supplement, every change in routine matters. That’s why so many people start taking Coenzyme Q10 - hoping it might help lower their pressure, reduce side effects from statins, or just feel better. But here’s the problem: mixing CoQ10 with your blood pressure meds isn’t as simple as popping a capsule with breakfast. Some people see real benefits. Others end up dizzy, with blood pressure dropping too low. And doctors? They’re still arguing about whether it even works.
What Is Coenzyme Q10, Really?
Coenzyme Q10, or CoQ10, isn’t some new-age wonder supplement. It’s a compound your body naturally makes - found in every cell, especially in your heart, liver, and kidneys. Think of it as a tiny battery charger for your cells. It helps turn food into energy and fights off damaging free radicals. Your body makes plenty when you’re young, but production drops as you age, especially if you’re on statins. That’s why many people start taking it - not because they’re sick, but because they feel a little drained.
Most supplements come in two forms: ubiquinone (the oxidized version) and ubiquinol (the reduced, more absorbable form). Ubiquinol is about 2 to 4 times better absorbed, which means you might need less of it to get the same effect. Doses range from 30 mg to 600 mg daily. Studies show that after 12 weeks of taking 100-200 mg per day, blood levels of CoQ10 can jump from around 0.5 μg/mL to over 2.5 μg/mL. That’s a big change.
Does CoQ10 Actually Lower Blood Pressure?
The short answer? Sometimes. But not for everyone, and not always in a way that matters.
A 2019 meta-analysis of 43 clinical trials found that CoQ10 lowered systolic blood pressure by an average of 3.5 mmHg. That sounds small - until you realize that just a 5 mmHg drop can cut stroke risk by 14%. But here’s the catch: those studies were messy. Some used tiny groups. Others didn’t control for diet or activity. One famous 1990 study claimed a 17.8 mmHg drop - but it was later dismissed by Cochrane reviewers because the numbers looked too perfect.
What’s clearer? The effect seems to show up after 10 to 14 days of daily use. And it’s dose-dependent. People taking under 200 mg/day saw bigger drops than those on higher doses. Longer trials - over 8 weeks - showed more consistent results. So if you’re thinking about trying it, give it at least two months before deciding.
Here’s Where It Gets Dangerous
CoQ10 doesn’t interact with blood pressure meds the way antibiotics or grapefruit juice do. It doesn’t block liver enzymes or speed up metabolism. But it doesn’t need to. It works on the same system - your blood vessels and heart muscle.
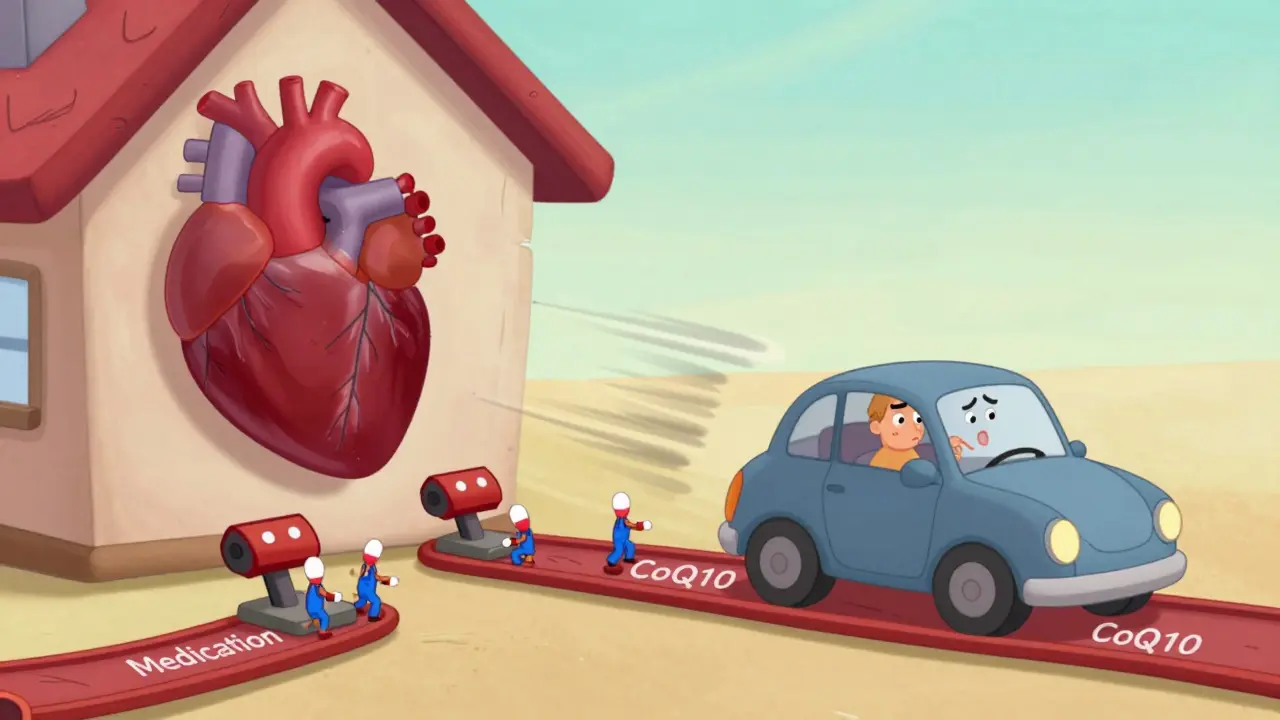
Imagine your blood pressure meds are like brakes. CoQ10? It’s like adding a little extra pressure to the brake pedal. Not enough to stop the car, but enough to make it feel like you’re braking harder than you meant to. That’s why some people end up with dizzy spells, fainting, or dangerously low pressure.
One case reported on Medscape in 2022 described a patient whose systolic pressure plunged to 85/55 after combining 300 mg of CoQ10 with lisinopril and hydrochlorothiazide. No doctor was involved. Just self-medication. That’s not a miracle - it’s a medical emergency.
And it’s not just about blood pressure. CoQ10 can interfere with warfarin, a blood thinner. Case reports in the Journal of Pharmacy Practice show INR levels dropping by 15-25% when CoQ10 is added. That means more clots, more risk of stroke. It’s not common - but it’s documented.
What Do the Experts Say?
There’s no consensus. And that’s the problem.
The American Heart Association says there’s not enough proof to recommend CoQ10 for high blood pressure. The European Food Safety Authority rejected a health claim for it back in 2011. Meanwhile, Japan approved CoQ10 as an adjunct treatment for hypertension in 1974 - and still uses it that way today.
Some doctors swear by it. Dr. Francisco Hernandez-Reyes, who led a 2007 study, found patients with isolated systolic hypertension had significant drops in pressure after taking CoQ10. Others, like the Cochrane team, call the evidence "very low quality" and warn against trusting those results.
But here’s what matters more than opinions: real-world behavior. On Drugs.com, 68% of users reported no issues. But 22% said they felt lightheaded. Reddit threads are full of stories like this: "After 4 months on 200mg CoQ10, my doctor cut my amlodipine from 10mg to 5mg - no problems."
That’s the gray zone. Not a miracle cure. Not a danger. But a tool that, in some cases, lets people reduce their meds.
Who Should Even Think About Taking It?
Not everyone. But if you fit one of these profiles, it’s worth a talk with your doctor:
- You’re on statins and feel tired or have muscle pain
- You have treatment-resistant hypertension (your pressure won’t budge even on three meds)
- You’re already on one or two blood pressure drugs and want to reduce dosage
- You’re not on warfarin or other blood thinners
Don’t take it if you’re pregnant, have low blood pressure already, or are on multiple antihypertensives without medical supervision. And never start it cold turkey while adjusting your meds.

How to Use It Safely
If you and your doctor decide to try CoQ10, here’s how to do it right:
- Start low: 100-200 mg per day. Avoid the 300-600 mg doses unless under supervision.
- Take it with food - especially fats. CoQ10 is fat-soluble. A peanut butter sandwich or avocado toast helps absorption.
- Wait 10-14 days before checking your pressure. The effect doesn’t happen overnight.
- Check your blood pressure twice a week. Keep a log. Bring it to your next appointment.
- Don’t stop or change your blood pressure meds without your doctor’s OK. CoQ10 isn’t a replacement.
- Watch for dizziness, fatigue, or unusually low readings. If your systolic drops below 100 consistently, call your provider.
Also - go for ubiquinol if you can afford it. It works faster and at lower doses. But don’t waste money on cheap brands. Look for third-party tested products (USP, NSF, or ConsumerLab certified).
The Bigger Picture
The CoQ10 market is worth over $1.2 billion. About 35% of sales are tied to heart health. But only 10% of those users are actually monitored by a doctor. Most are self-treating.
There’s a reason big pharma hasn’t made a CoQ10 pill for high blood pressure. The data is too inconsistent. It’s not a drug. It’s a supplement - which means no FDA approval, no standard dosing, no guarantees.
But that doesn’t mean it’s useless. For some, it’s a bridge - a way to reduce pills, feel more energy, and take back some control. For others, it’s a risk they didn’t know they were taking.
The truth? CoQ10 might help. But only if you treat it like medicine - not a vitamin.
Can CoQ10 replace my blood pressure medication?
No. CoQ10 is not a substitute for prescribed blood pressure medications. While some studies suggest it may help lower blood pressure slightly, it doesn’t work fast enough or consistently enough to replace drugs like lisinopril, amlodipine, or hydrochlorothiazide. Stopping your medication without medical supervision can be dangerous. If you’re considering reducing your dose, work with your doctor - don’t self-adjust.
How long does it take for CoQ10 to affect blood pressure?
Most people start to see changes in blood pressure within 10 to 14 days of daily use. But the full effect usually takes 4 to 8 weeks. Studies show that trials lasting longer than 8 weeks had more significant results. If you don’t notice any change after two months, it’s unlikely CoQ10 will help you - and you should talk to your doctor about other options.
Is CoQ10 safe with statins?
Yes - and that’s one of the most common reasons people take it. Statins lower CoQ10 levels in the body, which may contribute to muscle pain and fatigue. Supplementing with CoQ10 (typically 100-200 mg/day) can help reduce these side effects without interfering with the cholesterol-lowering effect of statins. There’s no evidence it reduces statin effectiveness. In fact, many cardiologists recommend it for statin users.
Can CoQ10 cause low blood pressure?
Yes - especially if you’re already on blood pressure medication. CoQ10 can have an additive effect, lowering pressure further. This is rare, but documented. Cases have been reported where systolic pressure dropped below 90 mmHg after combining CoQ10 with multiple antihypertensives. Symptoms include dizziness, fainting, or blurred vision. If you experience these, stop the supplement and check your pressure immediately. Always monitor your levels closely when starting CoQ10.
Does CoQ10 interact with warfarin?
Yes. CoQ10 may reduce the effectiveness of warfarin by lowering INR levels by 15-25%, according to case reports. This increases the risk of blood clots, stroke, or heart attack. If you’re on warfarin, do not take CoQ10 without close monitoring from your doctor. Regular INR tests are essential. Some providers will avoid CoQ10 entirely if you’re on blood thinners.
What’s the best form of CoQ10 for blood pressure?
Ubiquinol - the reduced, active form - is better absorbed than ubiquinone. Studies show it can raise blood levels 2-4 times higher at the same dose. For someone with high blood pressure, this means you might get the same effect with 100 mg of ubiquinol as you would with 200-400 mg of ubiquinone. It’s more expensive, but often more effective. Look for brands that specify "ubiquinol" on the label.

