Most people don’t talk about hemorrhoids - not because they’re rare, but because they’re embarrassing. The truth? About 75% of us will deal with them at some point in our lives. Whether you’re noticing bright red blood on the toilet paper, feeling a tender lump near your anus, or just can’t sit comfortably after a long day, you’re not alone. But here’s the thing: not all hemorrhoids are the same. And the treatment you need depends entirely on what kind you have.
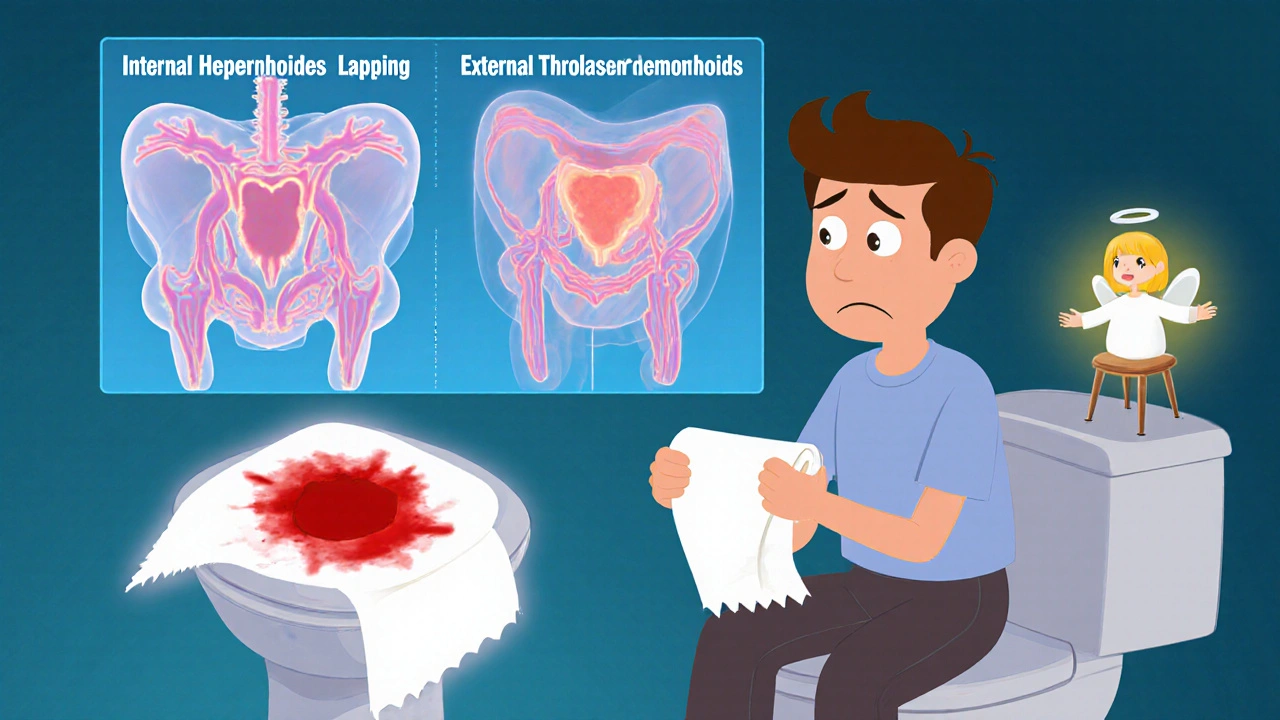
What’s the Difference Between Internal and External Hemorrhoids?
Hemorrhoids are just swollen veins - like varicose veins, but inside or around your anus. The key difference? Location. And that tiny detail changes everything about your symptoms and how you treat them.
Internal hemorrhoids form inside the rectum, above a line called the dentate line. This area has no pain receptors, so even when they swell, you might not feel pain at all. Instead, the main sign is bright red bleeding - usually seen on toilet paper, in the bowl, or on your stool. You might also feel like you haven’t fully emptied your bowels, or notice a soft bulge that comes out when you strain and then goes back in. These are graded from I to IV based on how far they prolapse:
- Grade I: Bleeds but doesn’t prolapse
- Grade II: Prolapses when you strain, but pops back in on its own
- Grade III: Comes out and needs to be pushed back in
- Grade IV: Stays out permanently and can’t be pushed back
External hemorrhoids form under the skin around the anus - right where there are lots of nerves. That’s why they hurt. You’ll feel itching, swelling, and a noticeable lump. If a blood clot forms inside (called a thrombosed hemorrhoid), it turns into a hard, purple or blue lump that feels like a marble under your skin. The pain hits fast and can be so intense you can’t sit down without wincing.
And yes, you can have both at the same time. That’s common. One might be bleeding silently inside, while another is throbbing outside. It’s easy to mix up the symptoms - which is why self-diagnosis often leads to the wrong treatment.
Why Do Hemorrhoids Happen?
Hemorrhoids aren’t caused by sitting too long on the toilet - at least not directly. They’re caused by pressure. Constant pressure on the veins in your rectum makes them stretch, swell, and bulge. The big culprits?
- Chronic constipation and straining during bowel movements
- Diarrhea that keeps you rushing to the bathroom
- Pregnancy - up to 35% of pregnant people get them, especially in the third trimester
- Obesity
- Heavy lifting
- Sitting for long periods, especially on the toilet
Here’s something most people don’t realize: your toilet habits matter more than you think. Sitting for more than 5 minutes on the toilet increases pressure on your rectal veins by about 30%. That’s why experts recommend using a small footstool to raise your knees above your hips - it mimics a squatting position and reduces strain. It’s simple, free, and works.
What Does the Bleeding Mean?
Any rectal bleeding sounds scary. And while hemorrhoids are the most common cause, they’re not the only one. You can’t assume it’s just hemorrhoids - especially if you’re over 50, have a family history of colon cancer, or notice changes in your bowel habits, weight loss, or dark, tarry stools.
Bleeding from hemorrhoids is bright red and fresh. It usually appears after a bowel movement. Bleeding from colon cancer, polyps, or inflammatory bowel disease can be darker, mixed with stool, or accompanied by other symptoms like cramping, fatigue, or unexplained weight loss. If you’re unsure, get it checked. Don’t wait. It’s not alarmist - it’s smart.
What Can You Do at Home?
For mild cases, you don’t need surgery or even a doctor’s visit. The first line of defense is simple, cheap, and backed by decades of evidence:
- Get more fiber. Aim for 25-30 grams a day. That’s 2 cups of cooked lentils, 1 cup of oats, 2 apples with skin, and a handful of almonds. Most people get less than half that. Fiber softens stool and reduces straining.
- Drink water. At least 8-10 glasses a day. Fiber without water makes stool harder - the opposite of what you want.
- Sitz baths. Sit in warm (not hot) water for 15-20 minutes, 2-3 times a day. It reduces swelling and soothes irritation. You can do this in a regular bathtub - no special kit needed.
- Avoid straining. If you don’t have a bowel movement after 5 minutes, get up. Walk around. Try again later.
- Use over-the-counter creams. Hydrocortisone cream (1%) can help with itching and swelling. Witch hazel pads (like Tucks) reduce inflammation. Avoid products with benzocaine or lidocaine - they can irritate the skin over time.
Don’t fall for “miracle cures” sold online. No cream, oil, or supplement can shrink hemorrhoids. Only lifestyle changes and medical treatments can.
When Do You Need Medical Treatment?
If home care doesn’t help after a week or two - or if symptoms get worse - it’s time to see a doctor. You don’t need to suffer in silence.
For internal hemorrhoids, doctors have several minimally invasive options:
- Rubber band ligation. A tiny rubber band is placed around the base of the hemorrhoid. It cuts off blood flow. The hemorrhoid shrinks and falls off in 5-7 days. It’s 90% effective for Grades I-III. You might feel pressure or mild cramping for a day or two.
- Sclerotherapy. A chemical solution is injected into the hemorrhoid. It causes scarring and shrinkage. Less effective than banding, but good for smaller ones.
- Infrared coagulation. A small probe delivers heat to the hemorrhoid, shrinking it. Pain is minimal, but you might need multiple sessions.
For thrombosed external hemorrhoids, timing matters. If you’re in severe pain and the lump is new (under 72 hours old), a simple procedure can help: the doctor makes a tiny cut, removes the clot, and the pain drops dramatically within minutes. After 72 hours, the clot starts to dissolve on its own - but the pain lasts longer.
For severe, recurring, or Grade IV hemorrhoids, surgery may be needed:
- Hemorrhoidectomy. The hemorrhoid is completely removed. It’s the most effective option - 95% success rate. But recovery takes 2-4 weeks. Pain is significant at first, so you’ll need prescription painkillers.
- Stapled hemorrhoidopexy. The prolapsed tissue is lifted back into place and stapled. Less pain than traditional surgery, but higher chance of recurrence.
Most people choose minimally invasive treatments first. Surgery is reserved for cases that don’t respond to anything else.

What Happens If You Ignore It?
Hemorrhoids don’t turn into cancer. But they don’t just go away on their own either. If you keep straining, keep eating low-fiber food, and keep sitting too long on the toilet, they’ll get worse. Internal hemorrhoids can prolapse permanently. External ones can become thrombosed, infected, or ulcerated.
And here’s the hidden cost: embarrassment. A survey by Heritage Surgical Group found that 68% of people waited over six months before seeing a doctor. By then, the problem was often much harder to treat. You don’t need to wait. Doctors have seen it all. They’re not judging you.
How to Prevent Them From Coming Back
Even after treatment, hemorrhoids can return - especially if you don’t change your habits. Studies show recurrence rates drop from 50% to just 5-10% when people stick to these basics:
- Keep eating 25-30g of fiber daily
- Drink water consistently - don’t wait until you’re thirsty
- Move your body. Walk 20-30 minutes most days. Exercise helps prevent constipation.
- Don’t hold it in. Go when you feel the urge.
- Use the footstool trick. It’s not a gimmick - it’s biomechanics.
- For pregnant people: sleep on your left side. It reduces pressure on pelvic veins.
These aren’t just “good habits.” They’re medical necessities if you’ve had hemorrhoids before.
When to See a Doctor Right Away
Don’t wait. Call your doctor if you have:
- Heavy or persistent bleeding
- Dizziness, weakness, or pale skin (signs of significant blood loss)
- Severe pain that doesn’t improve with home care
- Changes in bowel habits - like new constipation, diarrhea, or narrow stools
- Unexplained weight loss
- Symptoms that return after treatment
It’s not about being dramatic. It’s about ruling out something more serious. Your gut health matters.
Can hemorrhoids go away on their own?
Small, mild hemorrhoids can shrink on their own with proper diet, hydration, and sitz baths - usually within a week or two. But they won’t disappear completely unless the root cause (like constipation or straining) is fixed. Without lifestyle changes, they almost always come back.
Is it safe to use over-the-counter creams long-term?
Hydrocortisone cream (1%) is safe for short-term use (up to a week). Longer use can thin the skin around the anus. Witch hazel pads are gentler and can be used longer. Avoid numbing creams with lidocaine or benzocaine - they can irritate the area and mask symptoms that need medical attention.
Do hemorrhoids mean I have colon cancer?
No, hemorrhoids do not cause cancer. But rectal bleeding can be a symptom of colon cancer, polyps, or inflammatory bowel disease. If you’re over 50, have a family history, or notice other symptoms like weight loss or changes in bowel habits, get checked. Never assume bleeding is just hemorrhoids.
Can pregnancy cause hemorrhoids?
Yes. Up to 35% of pregnant people develop hemorrhoids, especially in the third trimester. Increased pressure from the growing uterus and hormonal changes relax the veins. Constipation from prenatal vitamins adds to it. Most improve after delivery, but managing fiber, water, and avoiding straining helps during pregnancy.
What’s the best way to prevent hemorrhoids?
Three things: eat 25-30g of fiber daily, drink enough water, and don’t sit on the toilet longer than 5 minutes. Use a footstool to raise your knees. Walk regularly. Don’t ignore the urge to go. These simple habits prevent 90% of cases.
If you’ve been ignoring symptoms because you’re embarrassed, stop. Hemorrhoids are common, treatable, and nothing to be ashamed of. The sooner you act, the less invasive the treatment. Your body is telling you something - listen to it.


9 Comments
JAY OKE
Been dealing with this for months. Sitz baths and fiber changed everything. No more pain, no more fear of the toilet. Just plain old common sense.
Rachel Whip
So many people don’t realize hemorrhoids aren’t a moral failing-they’re a biomechanical issue. The footstool trick? It’s not a gimmick. It’s physics. Your body wasn’t designed to squat on a porcelain throne. Also, stop wiping like you’re scrubbing a pan.
Hydrocortisone cream for itching, yes. Lidocaine for pain? No. That’s like putting duct tape on a leaking pipe.
And if you’re pregnant? You’re not broken. You’re just carrying a tiny human who’s pressing on your plumbing. Left-side sleeping helps. So does not holding it in.
Stop Googling ‘miracle hemorrhoid cures.’ There are none. Only consistency. Fiber. Water. Movement. Repeat.
I’ve seen patients wait two years because they were embarrassed. By then, it’s banding or worse. Don’t be that person.
Doctors have seen it all. We’ve seen worse. We don’t judge. We just want you to sit comfortably again.
And if you’re over 50 and bleeding? Get a colonoscopy. Not because you’re scared. Because you’re smart.
It’s not embarrassing. It’s human.
Ali Miller
Let me be the first to say this: AMERICA ISN’T DOING THIS RIGHT. We’ve got a $12 billion hemorrhoid cream industry built on lies and placebo. Meanwhile, the British NHS just gives you a leaflet and says ‘eat more beans.’ Guess what? It works. We need to stop selling snake oil and start teaching basic biology.
Also, why are we still sitting on toilets? We evolved to squat. The Romans knew this. The Chinese knew this. We’re the only ones who think sitting for 20 minutes while scrolling TikTok is normal.
And don’t get me started on ‘natural remedies’ sold by influencers with 300K followers who’ve never held a stethoscope.
Joe bailey
Man, this post is a lifesaver. I thought I was the only one who had this problem. Just started using the footstool and honestly? Game changer. Feels like my body finally remembers how to work right.
Also, I’ve been drinking more water and eating lentils like they’re going out of style. No more straining. No more panic when I feel that itch. Just… peace.
Thanks for saying it like it is. No fluff. Just facts. That’s rare these days.
Sanjay Menon
While your post is technically accurate, it lacks a nuanced ontological framework for understanding anorectal pathology within the context of late-stage capitalist bodily alienation. The hemorrhoid, as a somatic manifestation of bourgeois sedentary hegemony, is symptomatic of a deeper epistemic rupture between the body and its environment. You recommend fiber? How quaint. Have you considered the phenomenological implications of defecation as a colonial act?
Also, ‘sitz bath’ is a euphemism for bourgeois hygiene fetishism. I’ve been using cold seawater immersion since 2017. Much more aligned with ancestral wisdom.
Brittany Medley
Thank you for this. So many people think hemorrhoids are ‘just a thing you live with.’ They’re not. They’re a sign. And ignoring them doesn’t make them go away-it just makes them worse.
Also, if you’re using numbing creams long-term? You’re masking the problem. That’s like taking ibuprofen for a broken bone and calling it a day.
And yes-yes!-the footstool. It’s not a ‘hack.’ It’s biomechanics. Your colon doesn’t care about your IKEA chair. It cares about alignment.
And if you’re pregnant? You’re not weak. You’re growing a human. Be gentle with yourself.
And if you’re over 50? Get checked. Please. I’ve seen too many people wait until it’s too late.
Kaushik Das
Bro, I used to think hemorrhoids were some kind of punishment for eating too much spicy food. Then I found out it was just me sitting on the toilet scrolling memes for 15 minutes after every meal. Changed that. Now I do 5 minutes max. No phone. Just breathe. And boom-no more burning. Also, I started eating 2 cups of dal a day. My poop now has the texture of a baby’s butt. Perfect.
And yeah, the footstool? I used a stack of old books. Works like magic. No need to buy some fancy gadget.
Also, I used to feel so ashamed. Now I just tell my friends: ‘Hey, I got a little plumbing issue. Fixed it with lentils and posture.’ They laugh. Then they ask for the recipe.
mohit passi
Life’s too short to suffer in silence. 🌱💧🪑
Aaron Whong
The hemorrhoid, as a pathological artifact of the post-industrial defecatory regime, represents a semiotic rupture in the corporeal hermeneutic. The very act of ‘treatment’ reinforces the Cartesian dualism between body and self. True liberation lies not in rubber band ligation, but in the ontological reclamation of the squat-pre-civilizational, pre-capitalist, pre-toilet.
Moreover, the normalization of ‘fiber’ as a medical intervention is a symptom of the pharmakon economy. Fiber is not a cure-it is a pacifier for the colonized gut.
Perhaps the real question is not ‘how do we treat hemorrhoids?’ but ‘how do we dismantle the infrastructure that produces them?’