Skeletal Muscle Condition Staging Guide
Select a stage below to learn about symptoms, physiology, and typical treatments:
Acute Phase
Minutes to days
Sub-Acute Phase
Days to weeks
Chronic Phase
Weeks to years
Recovery Phase
Ongoing
Select a stage to view details
Click on any stage card above to see detailed information about symptoms, physiology, and treatment options.
Quick Symptom Tracker
Use this to assess your current condition stage:
When you hear the term skeletal muscle conditions is a group of disorders that affect the muscles attached to the skeleton, causing weakness, pain, or loss of function, it can feel overwhelming. Understanding skeletal muscle conditions can help you navigate symptoms, know what to expect at each stage, and work with healthcare providers for better outcomes.
Key Takeaways
- Most muscle conditions follow identifiable stages: acute, sub‑acute, chronic, and recovery.
- Early signs often include pain, swelling, and reduced strength; later stages may add fibrosis or permanent loss.
- Accurate staging guides treatment-rest and ice for early strains, medication for inflammatory diseases, and rehab for chronic phases.
- Common conditions (muscle strain, myositis, muscular dystrophy, atrophy, sarcopenia, rhabdomyolysis) share similar stage patterns but differ in causes and timelines.
- Regular assessment and tailored exercise programs can slow progression and improve quality of life.
What Is a Skeletal Muscle Condition?
A skeletal muscle condition refers to any disorder that impairs the contractile function of muscles attached to bones, leading to weakness, pain, or functional limitation. These conditions range from acute injuries like strains to chronic diseases such as muscular dystrophy. While the underlying causes vary-mechanical overload, genetic mutations, autoimmune attacks-the body’s response often follows a similar progression.
Common Types and Their Typical Stages
Below is a quick look at seven frequently encountered muscle conditions and how clinicians usually break them down into stages.
- Muscle Strain an overload injury that tears muscle fibers, typically graded I‑III based on severity
- Muscular Dystrophy a group of genetic disorders causing progressive muscle degeneration and weakness
- Myositis inflammatory muscle disease, often autoimmune, leading to muscle pain and swelling
- Muscle Atrophy loss of muscle mass due to disuse, denervation, or systemic illness
- Sarcopenia age‑related decline in muscle mass and strength, affecting up to 20% of adults over 65
- Rhabdomyolysis rapid breakdown of muscle fibers releasing myoglobin into the bloodstream, risking kidney injury
- Muscle Hypertrophy an adaptive increase in muscle size from resistance training, often used as a benchmark for healthy growth
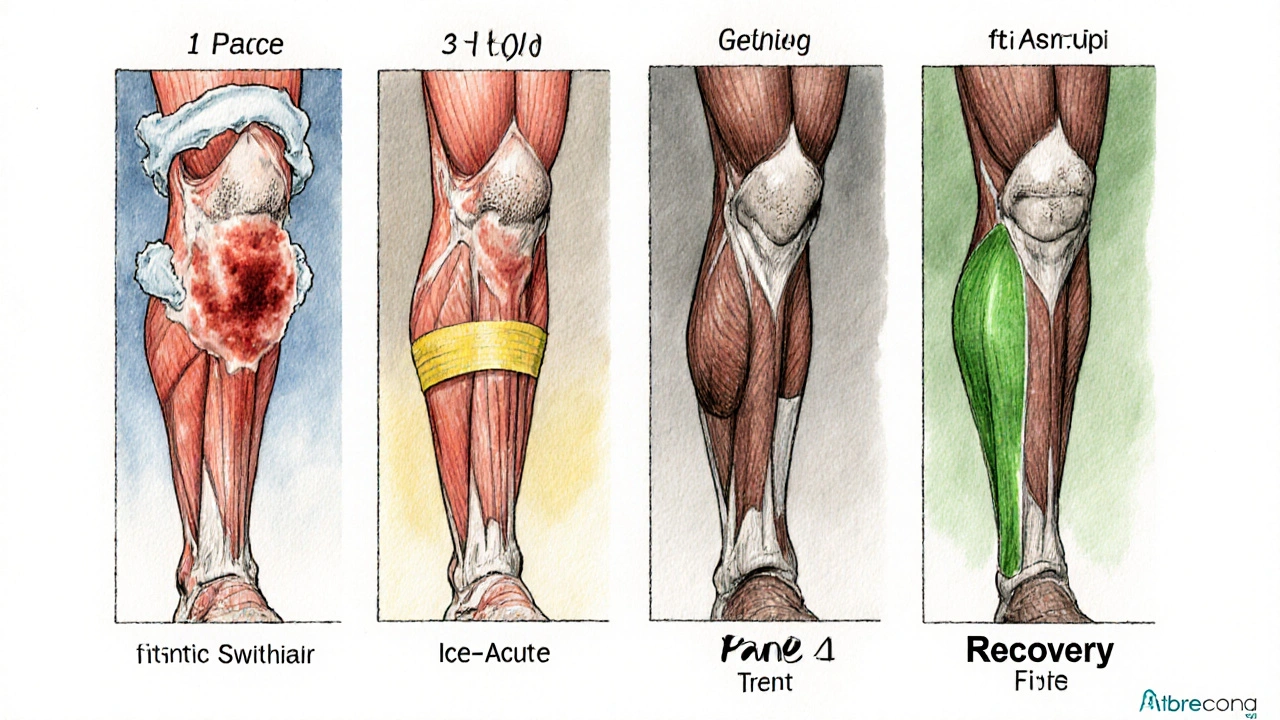
Stage‑by‑Stage Breakdown
Even though each condition has its quirks, clinicians often describe four overlapping phases. Recognizing which phase you’re in helps you pick the right interventions.
1. Acute (Early) Phase
Time frame: minutes to days after onset.
- Symptoms: sharp pain, swelling, bruising, reduced range of motion.
- Physiology: inflammatory cascade releases cytokines (IL‑6, TNF‑α), increasing vascular permeability.
- Typical actions: RICE (rest, ice, compression, elevation), NSAIDs, limited movement.
2. Sub‑Acute (Progressive) Phase
Time frame: several days to 2‑3 weeks.
- Symptoms: dull ache, stiffness, mild weakness.
- Physiology: fibroblast activity starts laying down collagen; for inflammatory diseases, immune cells infiltrate muscle tissue.
- Typical actions: gentle stretching, start of physiotherapy, possible corticosteroid pulses for autoimmune myositis.
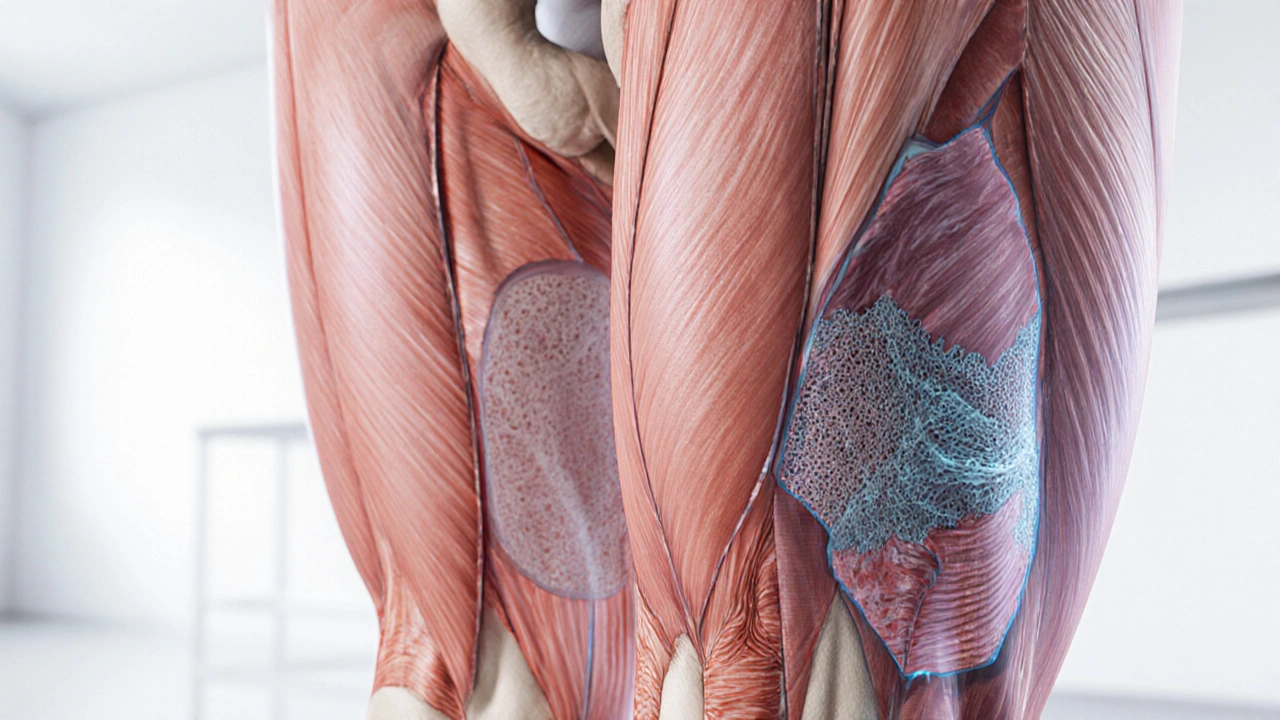
3. Chronic (Late) Phase
Time frame: weeks to months or years.
- Symptoms: persistent weakness, reduced muscle bulk, fatigue.
- Physiology: fibrosis replaces healthy fibers; in genetic conditions, ongoing degeneration outpaces regeneration.
- Typical actions: targeted strength training, disease‑modifying drugs (e.g., exon‑skipping therapy for Duchenne), nutritional support (protein, vitamin D).
4. Recovery / Maintenance Phase
Time frame: variable, often ongoing.
- Goals: regain functional strength, prevent re‑injury, slow progression.
- Tools: progressive resistance exercises, aerobic conditioning, regular monitoring (MRI, CK levels for myositis).
Comparison of Stages Across Common Conditions
| Condition | Acute Signs | Sub‑Acute Signs | Chronic Signs | Typical Treatment |
|---|---|---|---|---|
| Muscle Strain | Pain, swelling, limited use | Stiffness, mild weakness | Scar tissue, reduced flexibility | RICE → physio → graded loading |
| Muscular Dystrophy | Often no acute pain; early motor delay | Progressive weakness, gait changes | Significant muscle loss, contractures | Gene‑specific drugs, steroids, assisted devices |
| Myositis | Rapid onset of painful swelling | Persistent ache, elevated CK levels | Fibrosis, chronic fatigue | Immunosuppressants, physiotherapy, diet |
How to Self‑Assess Your Stage
- Track pain intensity. Use a 0‑10 scale three times a day; sudden spikes usually mean you’re still in the acute phase.
- Measure range of motion. Compare daily to baseline; loss >20% suggests sub‑acute or chronic.
- Check strength. Perform a simple grip‑or‑leg‑press test; a drop of more than 30% from usual indicates chronic involvement.
- Monitor biomarkers. If you have a diagnosis like myositis, record blood creatine kinase (CK) weekly; steady decline shows improvement.
- Seek professional evaluation. When pain persists >2 weeks, swelling isn’t reducing, or strength falls sharply, schedule a physio or physician visit.
Practical Tips for Each Phase
Acute: keep the area elevated, apply ice for 15‑20 minutes every 2‑3 hours, avoid heavy lifting.
Sub‑Acute: start gentle static stretching, incorporate low‑impact cardio (swimming, cycling) to promote circulation.
Chronic: focus on progressive resistance (e.g., 3 sets of 8‑12 reps), consider hiring a certified strength coach familiar with medical conditions.
Recovery/Maintenance: schedule monthly check‑ins, maintain a balanced diet with 1.2‑1.5g protein per kg body weight, stay hydrated to support muscle metabolism.
When to Call a Doctor
- Severe pain that isn’t relieved by NSAIDs.
- Dark urine (possible rhabdomyolysis).
- Rapid loss of muscle strength over days.
- Persistent swelling or fever, indicating infection.
- Difficulty breathing or swallowing (signs of severe myositis).
Future Directions in Muscle Care
Research in 2025 highlights two promising avenues:
- Gene‑editing therapies. CRISPR‑Cas9 trials for Duchenne muscular dystrophy report 30% increase in functional muscle mass.
- Targeted anti‑fibrotic drugs. Molecules that block TGF‑β signaling reduce scar tissue formation in chronic myositis.
While still experimental, these advances could shift the chronic phase from inevitable decline to manageable stability.
Frequently Asked Questions
How long does the acute phase last for a typical muscle strain?
The acute phase usually resolves within 3‑7 days if proper rest and ice are applied. Pain that persists beyond a week may indicate a higher‑grade strain or early chronic changes.
Can exercise worsen muscular dystrophy?
Moderate, supervised resistance training can actually preserve muscle function. Over‑exertion or high‑impact activities, however, may accelerate fiber damage.
What lab test is most useful for tracking myositis?
Serial creatine kinase (CK) measurements are standard. A steady decline after treatment signals reduced muscle inflammation.
Is swelling always a sign of injury?
Not always. Swelling can result from fluid retention, infection, or autoimmune activity. Context-pain level, temperature, and recent activity-helps differentiate the cause.
How can I prevent sarcopenia as I age?
Combine resistance training at least twice weekly with adequate protein intake (1.2‑1.5g/kg) and ensure vitamin D levels stay above 30ng/mL. Regular mobility work also preserves joint health.

15 Comments
Shaquel Jackson
Thanks for the info, but it feels like a snooze fest 😒
Tom Bon
Thank you for providing such a comprehensive overview of skeletal muscle pathology. The delineation of each phase, from acute to recovery, offers clinicians a clear framework for assessment and intervention. Incorporating both physiological mechanisms and treatment modalities enhances its utility for both practitioners and patients alike.
Clara Walker
While this guide appears thorough, it's clear that the pharmaceutical industry funded it to promote costly drug therapies over natural recovery methods. They've hidden the simple truth that most muscle injuries resolve with proper nutrition and rest without the need for expensive medications.
Jana Winter
The previous comment is well‑intentioned, yet it contains several stylistic inconsistencies. For instance, the phrase “both physiological mechanisms and treatment modalities” is redundant; the word “both” already implies a pair. Additionally, consider using the Oxford comma for clarity.
Linda Lavender
The skeletal muscle condition staging guide, as presented, unfurls a tapestry of clinical nuance that beckons the discerning reader. In its opening salvo, the author deftly categorizes the temporal evolution of muscular injury, deploying evocative icons to anchor each phase in the collective psyche. The acute phase, delineated as “minutes to days,” is aptly described with the classic triad of sharp pain, swelling, and restricted range of motion, evoking a visceral image of tissue trauma. Transitioning into the sub‑acute interval, the narrative gracefully acknowledges the shift toward dull ache and the nascent processes of collagen deposition, a subtle reminder of the body’s inherent reparative ambition. The chronic stage, however, is where the discussion attains a somber gravitas, illuminating the inexorable march of fibrosis and the attendant decline in muscle bulk, a lamentable fate for the afflicted. Yet, the guide does not surrender to nihilism; it offers a compass of therapeutic strategies ranging from RICE to exon‑skipping, thereby empowering clinicians with a repertoire of options. One cannot overlook the meticulous inclusion of emerging modalities such as CRISPR‑Cas9 gene editing, which hints at a future where genetic maladies may be coaxed back into equilibrium. Moreover, the emphasis on nutritional support-protein, vitamin D, and the like-underscores the interdisciplinary nature of musculoskeletal care. The integration of practical tips, such as progressive resistance training parameters, further bridges the gap between theory and bedside implementation. Of particular note is the attention to monitoring modalities; serial CK measurements and MRI surveillance provide objective anchors in an otherwise subjective landscape. The author’s commitment to patient education shines through in the readily accessible symptom tracker, which invites active self‑assessment and fosters a sense of agency. While the guide is replete with strengths, a critical eye discerns a paucity of discussion regarding comorbidities such as diabetes, which can profoundly alter healing trajectories. Additionally, the absence of culturally tailored rehabilitation protocols may limit its applicability in diverse populations. Nevertheless, the compendium stands as a commendable synthesis of current knowledge, marrying pathophysiology with pragmatic intervention. In sum, readers are left with both a granular understanding of each phase and a roadmap for navigating the treacherous waters of chronicity. The guide, therefore, constitutes a valuable resource for both novice and veteran practitioners alike.
Jay Ram
Great breakdown! Your detail really helps visualize each stage and the practical tips are golden. Keep it up!
Elizabeth Nicole
It's worth noting that early mobilization, when done correctly, can actually shorten the acute phase by promoting circulation and preventing stiffness. Combining low‑impact cardio, like swimming, with gentle stretching can accelerate recovery without overloading the injured tissue. Also, staying hydrated supports metabolic processes essential for tissue repair.
Dany Devos
The preceding comment provides useful advice; however, it would benefit from citing specific studies that substantiate the claim regarding early mobilization. References to peer‑reviewed literature enhance credibility and guide readers toward evidence‑based practices.
Sam Matache
Wow, this guide reads like a textbook for muscle nerds-way too much jargon for a simple strain. Who even needs CRISPR when you can just ice it?
Hardy D6000
Contrary to popular belief, dismissing emerging therapies ignores the very advancements that have transformed outcomes for many patients. The guide's inclusion of gene editing reflects real progress, not hype.
Amelia Liani
I appreciate how the guide balances scientific detail with actionable steps, making it accessible for patients navigating their own recovery journeys. The emphasis on monitoring and regular check‑ins shows real compassion.
shikha chandel
Indeed, patient‑centered care is paramount; brevity and clarity enhance adherence.
Zach Westfall
Listen folks this is the real deal no more half‑hearted advice get your protein up stay active and you’ll beat the odds
Pranesh Kuppusamy
One might argue that the pursuit of muscular health mirrors the broader quest for equilibrium within the self, wherein the interplay of inflammation and repair reflects the dialectic of conflict and resolution.
Crystal McLellan
Don't be fooled, they want you to rely on supplements sold by big pharma while hiding the simple truth that sunlight and proper diet are enough to heal muscles.