When your child gets sick, you want the fastest, safest relief. That’s why many parents and doctors turn to generic drugs for children-they’re cheaper, widely available, and seem like a no-brainer. But here’s the truth: what works for adults doesn’t always work for kids. Generic drugs aren’t just smaller versions of adult pills. For children, especially those under 2, the differences in inactive ingredients, concentrations, and how their bodies process medicine can mean the difference between healing and hospitalization.
Why Generic Drugs Aren’t Always Safe for Kids
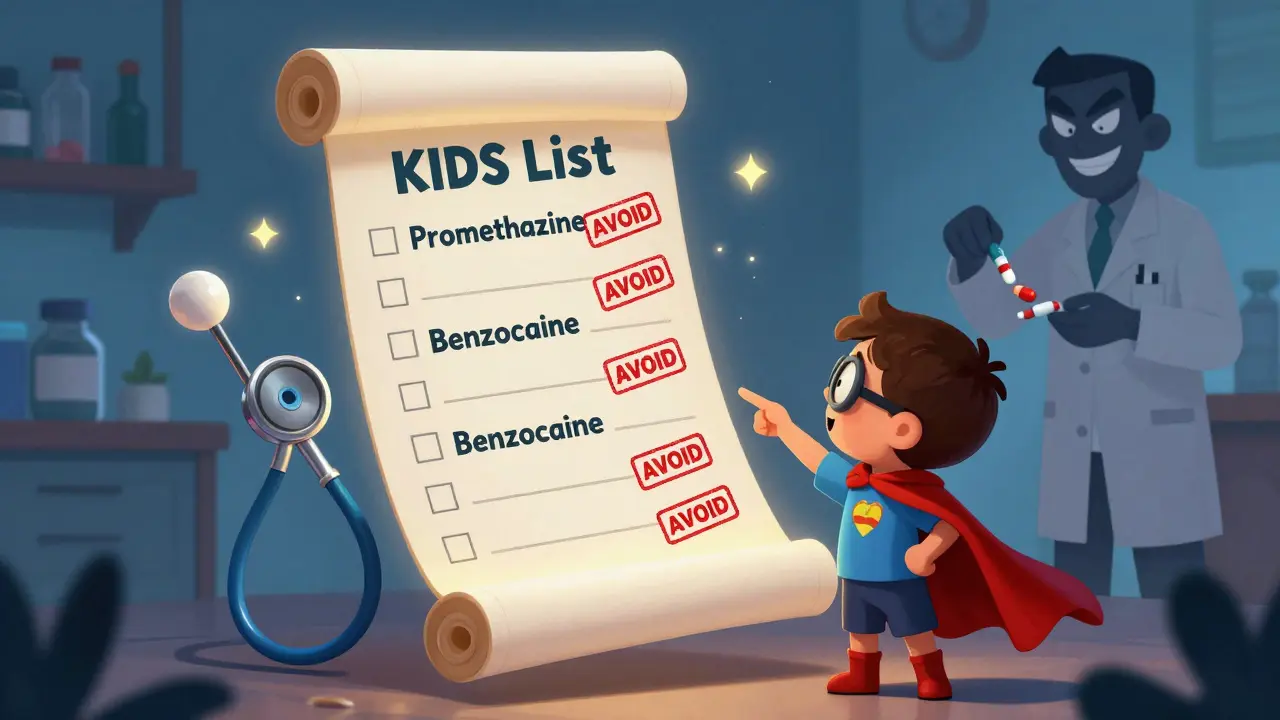
The FDA says generic drugs must have the same active ingredient as the brand-name version. That’s the law. But what they don’t require is the same inactive ingredients-things like dyes, preservatives, sweeteners, and fillers. For adults, these usually don’t matter. For babies and toddlers? They can be dangerous. Take benzocaine, a common generic topical anesthetic found in teething gels. Applied to a child’s mouth, it can cause methemoglobinemia-a rare but deadly condition where the blood can’t carry oxygen properly. The FDA warns against using it in children under 2. Yet, many parents don’t know the difference between the brand and the generic version on the shelf. Same goes for promethazine, a generic antihistamine. It’s been linked to fatal breathing problems in kids under 2. The KIDs List-a living guide from the Pediatric Pharmacy Association-flags it as an “avoid” drug for this age group. But if a doctor doesn’t specify “dispense as written,” a pharmacist might automatically swap the brand for the generic. No one checks. No one warns.The Hidden Risks: Formulations Matter More Than You Think
A child’s body isn’t a small adult. Their liver and kidneys are still developing. Their stomachs absorb drugs differently. Their brains are more sensitive to certain chemicals. That’s why even tiny changes in a drug’s formulation can cause big problems. For example, liquid versions of generic medications often come in different concentrations. One bottle might say 100 mg per 5 mL. Another, made by a different company, might say 125 mg per 5 mL. If a parent doesn’t check the label and uses the same syringe measurement, they could give their child 25% more medicine than intended. That’s enough to cause toxicity. Lidocaine viscous, a generic numbing gel for teething or mouth sores, carries the same warning: avoid under 2. Why? Because swallowing even a small amount can lead to seizures or slowed breathing. Yet, many parents think “it’s just a gel,” and use it because it’s cheaper. The FDA has issued multiple alerts on this, but awareness remains low. Topical steroids like betamethasone are another concern. Generic versions vary in strength-from medium to very high. Using a high-potency version on a baby’s diaper area for diaper rash can lead to adrenal suppression or Cushing syndrome. These aren’t theoretical risks. They’ve been documented in hospitals.The KIDs List: Your Secret Weapon Against Harm
The Pediatric Pharmacy Association’s KIDs List is the most comprehensive safety tool for pediatric drug use. It’s not a list of bad drugs-it’s a list of drugs that need caution or complete avoidance based on real-world harm. As of 2025, the list includes over 4,100 drugs with pediatric safety flags. Some are brand names. Most are generics. Each entry has a rating:- Avoid: Strong evidence of life-threatening risk. No exceptions.
- Caution: Risk exists, but benefit may outweigh it under close supervision.
- Promethazine → Avoid under 2, use caution up to 18
- Trimethobenzamide → Avoid in all patients under 18
- Linaclotide → Caution under 2 (risk of fatal dehydration)
- Guaifenesin → Avoid under 4
Off-Label Use Is the Norm-And It’s Risky
Here’s a startling fact: 40% of all medications given to children in the U.S. are used off-label. That means the drug wasn’t tested or approved for their age, weight, or condition. And 90% of those prescriptions are filled with generics. Why? Because most drugs aren’t studied in kids. The FDA’s Best Pharmaceuticals for Children Act and Pediatric Research Equity Act helped-but progress is slow. As of 2021, 60% of generic drugs still lack pediatric dosing info. Only 35% of brand-name drugs have the same gap. Doctors often guess the dose based on weight. But guessing is dangerous. A 10-fold dosing error-giving 10 times too much-isn’t rare. That’s why experts like Dr. John N. van den Anker insist on the “zero rule”: never write “1.0 mg.” Write “1 mg.” A decimal point can be missed. A zero can be added. And in a child, that’s fatal.What Parents Can Do Right Now
You don’t need a medical degree to protect your child. Here’s what works:- Ask for the brand if your child has had a reaction to a generic before. Say: “I need the brand-name version. My child had a reaction to the generic.”
- Check the concentration on every liquid medication. Write it down. Compare it to the last bottle.
- Use an oral syringe-never a teaspoon or shot glass. Household spoons vary by up to 50% in volume.
- Keep a current med list-all prescriptions, OTC, vitamins, herbal drops. Update it every time something changes.
- Never use adult medicine for a child. Even “a little bit” can be toxic.
- Turn on the lights when giving medicine. Most errors happen in dim light.
- Never use expired drugs or someone else’s prescription.
When to Say No to Substitution
Some drugs have a narrow therapeutic index-meaning the difference between a helpful dose and a toxic one is tiny. For these, generic substitution can be dangerous:- Levothyroxine (for hypothyroidism)
- Phenytoin (for seizures)
- Warfarin (blood thinner)
- Propranolol (for heart conditions or infantile hemangiomas)

What’s Changing in 2025 and Beyond
The FDA just issued new guidance in May 2024: generic drug makers must now include pediatric dosing information if it exists. Full compliance is required by December 2025. That’s a big step. The European Medicines Agency has already seen 78% compliance with pediatric testing rules. The U.S. is at 42%. But pressure is growing. Pediatric-specific formulations are growing at 6.2% a year. AI tools are being tested to predict safe doses for generics with 89% accuracy. Still, the biggest change won’t come from regulation. It’ll come from awareness.Real Stories, Real Consequences
On Reddit’s r/Pediatrics, a mother wrote: “My 3-year-old had severe diarrhea after switching from brand-name loperamide to generic. We thought it was a stomach bug. Turned out the filler in the generic was triggering his IBS.” Another parent on Nemours KidsHealth said: “My 5-month-old broke out in a rash after we switched to generic cetirizine. The preservative was different. We didn’t know it could do that.” Pharmacists report that 32% of medication errors they catch in pediatrics are due to inappropriate generic substitutions. Most involve liquids, antibiotics, or seizure meds. These aren’t outliers. They’re symptoms of a system that treats children like small adults.Final Thought: Safety Isn’t Cheap
Generic drugs save money. That’s good. But when it comes to children, safety shouldn’t be traded for savings. A $2 generic that causes a hospital visit costs more than a $20 brand-name drug that works safely the first time. Ask questions. Demand clarity. Use the KIDs List. Use an oral syringe. Know your child’s meds. The system isn’t perfect. But you can be the difference between a mistake and a tragedy.Are generic drugs always safe for children?
No. While generic drugs have the same active ingredient as brand-name versions, their inactive ingredients-like dyes, preservatives, and fillers-can differ and may cause allergic reactions, toxicity, or absorption issues in children. Some generics are not tested for safety in kids under 2, and dosing concentrations can vary between brands, increasing the risk of overdose.
What is the KIDs List and why should I use it?
The KIDs List (Key Potentially Inappropriate Drugs List) is a living guide from the Pediatric Pharmacy Association that identifies over 4,100 drugs with known safety risks for children. It classifies drugs as “avoid” or “caution” based on evidence of harm. It’s updated quarterly and includes both brand-name and generic drugs. Parents and providers should check it before giving any new medication to a child.
Can I substitute a generic for a brand-name drug without asking my doctor?
You shouldn’t assume substitution is safe. Many pediatric drugs, especially those with narrow therapeutic windows like levothyroxine or phenytoin, require the exact formulation. Always ask your doctor to write “dispense as written” on the prescription if you’re unsure. Pharmacists can legally substitute generics unless instructed otherwise.
Why are liquid medications riskier for kids?
Liquid medications often come in different concentrations (e.g., 100 mg/5 mL vs. 125 mg/5 mL), and parents may use household spoons instead of oral syringes, leading to 50% more dosing errors. A single wrong measurement can result in overdose, especially in infants. Always use the syringe provided, check the concentration on the label, and never guess.
What should I do if my child has a reaction to a generic drug?
Stop the medication immediately and contact your pediatrician or poison control. Note the drug name, dosage, and symptoms. Report the reaction to the FDA’s MedWatch program. Ask your doctor to prescribe the brand-name version going forward and write “dispense as written” on the prescription to prevent future substitutions.



10 Comments
Henriette Barrows
Just read this and my heart dropped. My daughter had a rash after we switched to a generic cetirizine-no one warned us. I thought generics were just cheaper versions of the same thing. Turns out, they’re not. I’m printing out the KIDs List and taping it to the fridge. Every parent needs to see this.
Teresa Rodriguez leon
This is why I stopped trusting pharmacists. They don’t care if your kid gets sick as long as they hit their quota.
Nisha Marwaha
The pharmacovigilance infrastructure in pediatric populations remains critically underdeveloped, particularly with regard to excipient-mediated adverse drug reactions. The KIDs List represents a paradigmatic shift in risk stratification, but dissemination remains hampered by fragmented clinician education and lack of EHR integration. We must advocate for mandatory pediatric-specific labeling protocols and real-time pharmacy alert systems to mitigate iatrogenic harm.
Paige Shipe
Why do people keep acting like kids are fragile little snowflakes? I gave my son generic Tylenol since he was 6 months old. He’s 12 now, healthy as a horse. You’re overcomplicating this. The FDA approves these drugs for a reason. Stop being paranoid.
Tamar Dunlop
As a mother of two, and a Canadian living in a country where pediatric drug safety is rigorously monitored, I must say-this article is nothing short of a clarion call. The fact that we allow pharmacists to substitute formulations without explicit consent is not just negligent-it is morally indefensible. Our children deserve better than cost-driven compromises. I will be sharing this with every pediatrician I know.
David Chase
OMG I KNEW IT!!! 😤🔥 Generic drugs are just corporate greed disguised as savings! My cousin’s kid had a seizure from a generic lidocaine gel-AND THE PHARMACY DIDN’T EVEN TELL THEM?!?!?!?!! THIS IS WHY AMERICA IS FALLING APART!! #StopGenericDangers #KidsAreNotSmallAdults
Duncan Careless
Interesting piece. I’ve worked in a pediatric ward for 14 years and seen too many dosing errors tied to liquid generics. The oral syringe point? 100% correct. We’ve started giving every parent a calibrated syringe with every prescription. Small thing, huge impact. Also, ‘dispense as written’ should be default for anything under 5. Just sayin’.
Samar Khan
LMAO at people panicking over fillers. 😂 My kid takes generic antibiotics every time he gets an ear infection. He’s fine. You’re all acting like this is a horror movie. Next you’ll say the water’s toxic because it has fluoride. Grow up.
Russell Thomas
Oh wow. So now we’re blaming the generic drug industry for every bad parenting decision? Let me guess-you also blame the microwave for your kid’s picky eating? 😏 The real problem? Parents who don’t read labels. Not the pharmacy. Not the FDA. YOU. Go read the bottle before you pour. It’s not that hard.
Amy Cannon
While the intent of this article is undoubtedly noble, and the anecdotal evidence presented is both poignant and compelling, one cannot overlook the broader systemic context in which pharmaceutical substitution occurs. The United States healthcare infrastructure, particularly in ambulatory pediatric care, remains profoundly under-resourced. Pharmacists, often overworked and underpaid, are not equipped to provide individualized counseling for every prescription-especially when insurance formularies incentivize substitution. Until we address the root causes of pharmaceutical accessibility and provider burnout, we risk creating a culture of fear rather than one of informed empowerment. The KIDs List is a vital tool, yes-but it must be paired with structural reform, not just parental vigilance. We cannot medicate systemic failure with individual responsibility.