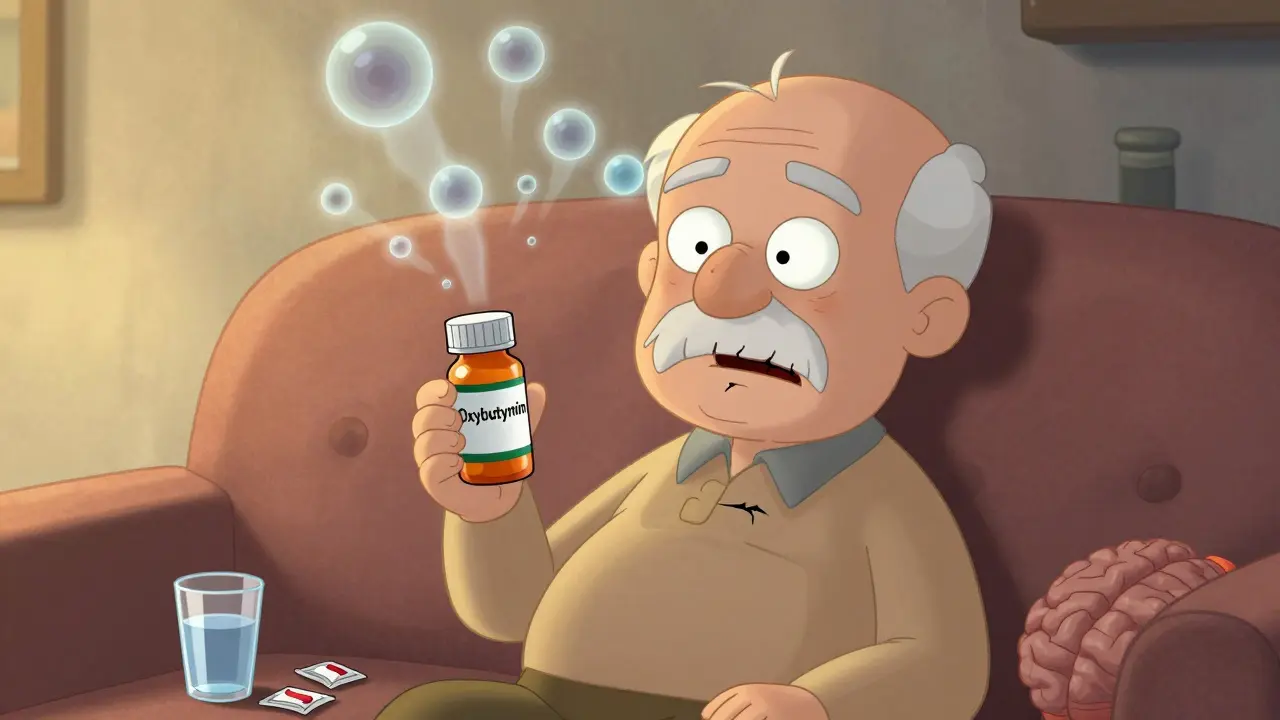
Many older adults take anticholinergic medications without realizing they could be slowly harming their brain. These drugs - found in common treatments for overactive bladder, allergies, depression, and Parkinson’s - block acetylcholine, a key chemical for memory and focus. What seems like a simple fix for one problem might be quietly setting the stage for another: memory loss, confusion, and even faster brain shrinkage.
What Are Anticholinergics and Why Are They So Common?
Anticholinergics are a class of drugs that stop acetylcholine from doing its job in the brain and body. Acetylcholine helps with learning, attention, muscle control, and saliva production. When you block it, you reduce symptoms like bladder spasms, excessive sweating, or tremors. But you also turn off important signals in the brain.
These drugs aren’t rare. About 1 in 3 older adults in the U.S. are taking at least one medication with anticholinergic effects. Common ones include:
- Oxybutynin (for overactive bladder)
- Diphenhydramine (Benadryl, for allergies and sleep)
- Amitriptyline (for depression and nerve pain)
- Trihexyphenidyl (for Parkinson’s)
They work. That’s why doctors still prescribe them. But the trade-off isn’t always clear to patients. And the longer you take them, the more your brain pays the price.
The Brain Changes You Can’t See
It’s not just feeling foggy. Brain scans show real, measurable damage. People taking high-anticholinergic drugs (rated 2 or 3 on the Anticholinergic Cognitive Burden scale) lose brain volume faster than those who don’t take them. One study of 451 older adults found they had:
- 0.5% to 1.2% more brain shrinkage per year
- 8% to 14% less glucose use in the hippocampus - the memory center
- 10% to 15% larger ventricles (fluid-filled spaces in the brain, which grow when brain tissue shrinks)
These changes aren’t just numbers on a scan. They show up in daily life. Users of high-burden anticholinergics performed 23% to 32% worse on memory tests and 18% to 27% worse on tasks requiring planning or focus. And it gets worse with time. Each extra point on the ACB scale added 0.3% more brain loss per year.
Dr. Shannon Risacher, who led one of the key studies, said: “These findings help explain how these drugs might push the brain toward dementia.” In her study, 63% of long-term users developed mild cognitive impairment or Alzheimer’s within 10 years - compared to 38% of non-users.
Dry Mouth Isn’t Just Uncomfortable - It’s a Warning Sign
If you’re constantly thirsty, chewing gum all day, or struggling to swallow food, your dry mouth isn’t just annoying. It’s a direct sign the drug is working - and working too hard.
Anticholinergics block acetylcholine in the salivary glands, reducing saliva by up to 70%. This isn’t a rare side effect. Eighty-two percent of users on Drugs.com report severe dry mouth. Some describe needing 2-3 liters of water daily just to speak or eat. Others say their tongue feels glued to the roof of their mouth.
But dry mouth does more than make life unpleasant. It increases the risk of:
- Tooth decay and gum disease
- Difficulty swallowing (which can lead to choking or pneumonia)
- Bad breath and mouth infections
It’s also a red flag. If you’re feeling this dry, your brain is likely being affected too - because the same mechanism causing dry mouth is also blocking signals in your memory centers.

Not All Anticholinergics Are Created Equal
Here’s the good news: you don’t have to take a high-risk drug if there’s a safer option.
Drugs are rated on the Anticholinergic Cognitive Burden (ACB) scale from 0 to 3:
- ACB 3 (High Risk): Scopolamine, diphenhydramine, oxybutynin
- ACB 2 (Medium Risk): Amitriptyline, tolterodine
- ACB 1 (Low Risk): Glycopyrrolate, trospium, darifenacin, tiotropium
- ACB 0 (No Risk): Mirabegron, solifenacin (low ACB), beta-3 agonists
For overactive bladder - one of the most common uses - oxybutynin (ACB 2-3) causes 28% more cognitive decline than tolterodine (ACB 1-2). But there’s an even better choice: mirabegron. It works just as well for bladder control, has zero anticholinergic effects, and doesn’t cause dry mouth or brain fog. The problem? It costs $350 a month. Generic oxybutynin? $15.
Many doctors still reach for the cheap option. But the long-term cost to your brain may be far higher.
When Stopping Isn’t Safe - And What to Do Instead
Some people need anticholinergics. If you have Parkinson’s and stop your medication suddenly, your tremors and stiffness can explode. Abruptly quitting amitriptyline can trigger severe withdrawal.
But that doesn’t mean you’re stuck. The goal isn’t always to quit - it’s to reduce risk.
Experts recommend:
- Using the lowest dose possible
- Taking it for the shortest time needed
- Switching to lower-ACB alternatives when available
- Monitoring cognition every 6 months with the MoCA test
For dry mouth, try sugar-free gum (boosts saliva by 30-40%), prescription saliva substitutes like Xerolube, or pilocarpine - a drug that actually stimulates saliva production. A 2018 NEJM study showed pilocarpine increased salivary flow by 50-70%.

What’s Changing in 2026 - And What You Should Know
The tide is turning. In 2022, the FDA required stronger warning labels on 12 high-risk anticholinergics. The UK’s NICE guidelines now recommend deprescribing these drugs in 68% of long-term users over 65. Medicare prescriptions for high-ACB drugs have dropped 22% since 2015.
Newer drugs are being designed to avoid the brain. Trospium chloride XR (Sanctura XR) has 70% less brain penetration than oxybutynin. Karuna Therapeutics’ xanomeline - being tested for Alzheimer’s psychosis - causes 40% less dry mouth than older antipsychotics.
And AI tools are stepping in. Systems like MedAware now flag risky prescriptions before they’re written. One study predicts these tools could prevent 200,000-300,000 dementia cases per year in the U.S. by cutting inappropriate prescriptions by half.
What to Do Now
If you or someone you care about is on an anticholinergic, ask these questions:
- What’s the ACB score of this medication?
- Is there a non-anticholinergic alternative? (Like mirabegron for bladder issues)
- Can we try a lower dose or switch to a low-ACB version?
- Have we checked cognitive function in the last 6 months?
- Are we managing dry mouth - not just ignoring it?
Don’t stop medication on your own. But do ask. Your brain is worth the conversation.
Do all anticholinergics cause dementia?
No, not all. But long-term use of high-ACB drugs (scores 2-3) is strongly linked to increased dementia risk. Studies show users of these drugs have up to double the risk after 3+ years. Lower-ACB drugs (score 1) show little to no cognitive impact. The key is the dose, duration, and specific drug - not the whole class.
Can dry mouth from anticholinergics be reversed?
Yes, often. Once you stop or reduce the medication, saliva production usually returns within days to weeks. In the meantime, sugar-free gum, staying hydrated, and prescription products like pilocarpine or Xerolube can help manage symptoms. But if dry mouth persists after stopping the drug, see a dentist or doctor - it could signal another issue.
Is it safe to take diphenhydramine (Benadryl) for sleep?
Not for long-term use, especially over 65. Diphenhydramine is an ACB 3 drug - the highest risk category. Studies link it to faster brain shrinkage and memory decline. It’s also linked to next-day drowsiness and falls. Safer sleep options include melatonin, cognitive behavioral therapy for insomnia (CBT-I), or low-dose trazodone - none of which carry anticholinergic risks.
What’s the best alternative to oxybutynin for overactive bladder?
Mirabegron is the top alternative. It works as well as oxybutynin but has no anticholinergic effects, so it doesn’t cause brain fog or dry mouth. Behavioral changes like timed voiding and pelvic floor exercises are also effective and risk-free. If those don’t work, low-ACB options like darifenacin or trospium are safer than oxybutynin.
How do I find out if my medication has anticholinergic effects?
Ask your pharmacist or doctor for the Anticholinergic Cognitive Burden (ACB) score. You can also check the Anticholinergic Burden Scale online - many are freely available. Look up your drug by name. If it’s rated 2 or 3, ask if a lower-risk option exists. Don’t rely on the label - many drugs don’t clearly warn about cognitive risks.
Can cognitive decline from anticholinergics be reversed?
Some improvement is possible after stopping the drug, especially if it’s been used for less than a few years. Memory and attention tests often show gains within 3-6 months. But if brain shrinkage has been ongoing for 5+ years, some damage may be permanent. The earlier you act, the better your chances of recovery.

12 Comments
Paul Barnes
Just read this and immediately checked my meds. Oxybutynin. ACB 3. Shit.
Already forgetting where I put my keys. Guess I’m not just getting old.
Time to call my doctor tomorrow.
clifford hoang
THEY KNOW. THEY’VE ALWAYS KNOWN. 🤫
Big Pharma doesn’t care if your brain melts - they make more money selling you new pills for the side effects.
Dry mouth? Buy more water.
Memory loss? Buy more dementia drugs.
It’s a cycle, folks. 😈💊
They’re not just selling meds - they’re selling slow brain death. And you’re paying for it in cash. 🧠💸
Arlene Mathison
OMG I’ve been taking Benadryl for sleep for YEARS 😭
And now I’m realizing why I feel so foggy all the time.
But I’m not ready to quit cold turkey - any tips on how to wean off safely? I’m scared.
Also - thank you for writing this. I needed to hear it.
Carolyn Rose Meszaros
My grandma’s on amitriptyline and she’s been forgetting her own name lately…
She also drinks 3 liters of water a day and chews gum nonstop.
I showed her this article. She cried.
We’re scheduling a med review this week.
Thank you for giving us the language to talk about this.
❤️
Greg Robertson
Good stuff. I’m a nurse and I see this all the time.
Older patients are often prescribed these meds because they’re cheap and easy.
But nobody talks about the brain fog until it’s too late.
Just last week, a patient asked me why she couldn’t remember her grandkids’ birthdays.
Turned out she’d been on diphenhydramine for 8 years.
She didn’t know it was even an issue.
Education matters.
Nadia Watson
It is with profound concern that I must underscore the systemic negligence surrounding the prescription of anticholinergic agents in geriatric populations. The cognitive burden scale, while empirically validated, remains underutilized in clinical practice. Furthermore, the disparity between pharmaceutical cost and neurological consequence represents a moral failure in healthcare delivery. One must question the ethical imperative of prescribing ACB-3 agents when non-anticholinergic alternatives exist, even at higher monetary cost. The long-term societal burden of iatrogenic dementia is incalculable.
It is my hope that regulatory bodies will enforce mandatory ACB labeling on all OTC and prescription formulations, and that prescribers undergo continuing education in geriatric pharmacology. The time for complacency has passed.
Shane McGriff
Paul - you’re not alone. I switched from oxybutynin to mirabegron last year. Cost me $400 a month, but my brain feels like it’s been unplugged from a static shock.
And my dry mouth? Gone.
My wife says I’ve been talking more, laughing more - like my old self.
Don’t wait until you’re forgetting your kid’s name. Talk to your doctor. Even if it’s scary. You’ve got this.
Jacob Cathro
lol so now we’re blaming Big Pharma for people being lazy? 😂
People take Benadryl because it’s free on CVS coupons and they don’t wanna pay for CBT-I.
And now you want them to pay $350 for a bladder pill? Nah.
Also - brain shrinkage? My uncle took this stuff for 15 years and he’s still out here fixing his truck at 82. You’re just fearmongering.
Also - dry mouth? That’s just aging. Get a humidifier.
Stop making everything a crisis.
Thomas Varner
Wait - so mirabegron works as well as oxybutynin… but costs 20x more? That’s insane.
And the FDA only just added warnings in 2022? Why not 10 years ago?
Also - how many people even know what ACB means? I didn’t.
And why isn’t this on the pill bottle? Like, a big red warning?
It’s like they want us to be confused.
And then they profit from the dementia meds too. It’s a business model.
And now I’m paranoid about every cold medicine I’ve ever taken…
Art Gar
There is no such thing as 'anticholinergic cognitive burden.' This is a construct invented by neurologists to justify their own research grants. The studies cited are observational, riddled with confounding variables - including age, comorbidities, and polypharmacy. To isolate a single drug class as the primary driver of cognitive decline is scientifically unsound. Furthermore, the suggestion that patients should abandon proven, effective therapies in favor of expensive alternatives is not only impractical - it is ethically irresponsible. The burden of proof lies with those who claim causality - not with those who prescribe based on clinical experience.
Edith Brederode
My mom’s on trospium now - ACB 1 - and she’s doing way better.
Still a little dry mouth, but nothing like before.
She started doing pelvic floor exercises too - and honestly? She says she feels more in control.
Also - I got her a little humidifier and she sleeps better.
Small changes, big difference.
Thank you for this. I shared it with my whole family.
Emily Leigh
So… we’re supposed to just stop taking meds that work because some study says they might hurt our brain? What if I need them to function? What if I’d rather be dry-mouthed and lucid than wet-mouthed and confused? I’m not a lab rat. I’ve got a life. This feels like medical gaslighting.