When you hear that hepatitis C has been cured, it’s natural to think the danger is over. After all, the virus is gone. Your liver is healing. You feel better than you have in years. But here’s the hard truth: liver cancer risk after SVR doesn’t disappear - not even close.
Sustained Virologic Response (SVR) means the hepatitis C virus is undetectable in your blood 12 or 24 weeks after finishing treatment. That’s a win. Direct-acting antivirals (DAAs) cure more than 95% of people. But curing the virus doesn’t erase the damage it left behind. If you had advanced fibrosis or cirrhosis before treatment, your risk of developing liver cancer - hepatocellular carcinoma (HCC) - remains real. And it’s not small.
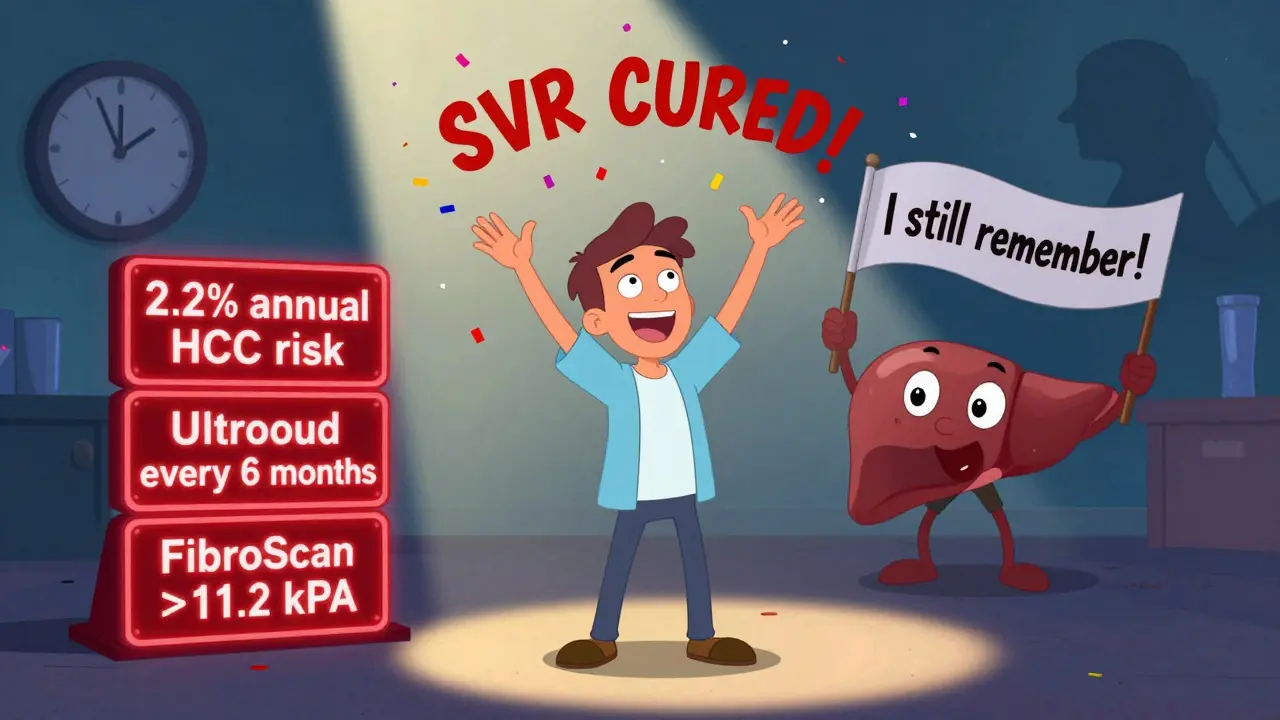
Studies show SVR cuts HCC risk by about 71%. That sounds impressive. But let’s put it another way: even after cure, people with cirrhosis still develop liver cancer at a rate of about 2.2 cases per 100 people each year. That’s more than 2% annually. Compare that to the general population, where HCC is rare. This isn’t theoretical. It’s happening in clinics right now.
Why the Risk Doesn’t Go Away
Your liver doesn’t reset to a clean slate after hepatitis C is gone. Years of inflammation, scarring, and cell damage don’t vanish overnight. Even when the virus is gone, the liver’s repair process can go off track. Molecular studies show that pathways tied to cell growth, inflammation, and adhesion stay activated long after SVR. One key protein, SPHK1, stays elevated in people who later develop HCC - even with no virus present.
Think of it like this: you put out a fire, but the ground is still hot. Smoldering embers can spark a new blaze. In your liver, those embers are the scar tissue, the altered DNA, the lingering immune signals. The virus is gone, but the environment it created still favors cancer.
This is why fibrosis stage matters more than anything else. If you had F3 (advanced fibrosis) or F4 (cirrhosis) before treatment, your risk stays high. If you had F0-F2 (mild or no scarring), your risk drops to nearly zero. That’s the dividing line. And it’s why guidelines disagree.
The Global Divide in Guidelines
Here’s where things get messy. In Europe, doctors are told to keep scanning every six months if you had advanced fibrosis or cirrhosis - even after SVR. The European Association for the Study of the Liver (EASL) says: “Don’t stop.”
In the U.S., the American Association for the Study of Liver Diseases (AASLD) says: “Only keep scanning if you still have cirrhosis.” They don’t recommend routine ultrasound for people with advanced fibrosis (F3) but no cirrhosis.
Why the difference? It’s not about who’s right. It’s about risk tolerance and real-world gaps. EASL worries that fibrosis can be misread. Ultrasound isn’t perfect. Some people thought to have F3 actually have early cirrhosis. And missing one HCC case can be deadly. AASLD argues that the absolute risk for F3 patients is too low to justify the cost and anxiety of lifelong scans.
But here’s what both sides agree on: if you had cirrhosis before treatment, you need ongoing surveillance. Period. The data is clear. Annual HCC risk above 1.32% means you’re in the high-risk zone. And that’s where most cirrhotic patients land - even after SVR.
How We Measure Risk Now
Doctors don’t guess anymore. They use tools. Two are widely used: FibroScan (transient elastography) and the FIB-4 index.
FibroScan measures liver stiffness. A reading above 11.2 kPa after SVR signals higher risk. Before treatment, the cutoff was 12.6 kPa. The fact that it dropped after cure? Good sign. But if it’s still above 11.2, you’re not out of the woods.
FIB-4 uses your age, platelet count, and liver enzyme levels. A score above 3.25 after SVR means you’re at increased risk. These aren’t perfect - but they’re better than nothing. And they’re non-invasive. No biopsy needed.
Some centers are starting to use the GALAD score - a blood test that combines gender, age, AFP, AFP-L3, and DCP. It’s 85% sensitive for spotting early HCC. Still mostly used in research, but it’s coming fast.
And now, new tools are emerging. Researchers at Massachusetts General Hospital are testing a dynamic model that tracks FibroScan results over time. Early data shows that if your stiffness drops below 9.5 kPa after SVR and stays there, you might safely extend your scans to once a year - or even longer.
The Big Problem: People Stop Getting Screened
Here’s the scary part: even when guidelines say to keep scanning, most people don’t.
A 2023 study found only about 25% of eligible patients get the recommended semiannual ultrasounds. Why? Because they think they’re cured. They feel fine. Their doctor doesn’t remind them. The system forgets them.
That’s the silent crisis. After years of battling hepatitis C, patients are told they’re free. They celebrate. They stop going to the doctor. They don’t realize the cancer risk is still there - just lower. And without screening, HCC grows silently. By the time symptoms show up, it’s often too late.
The Veterans Health Administration saw a 32% increase in screening rates after they added automated reminders to patient records. That’s not magic. That’s systems working.
What You Should Do Right Now
If you’ve achieved SVR, here’s what you need to know:
- If you had cirrhosis (F4) before treatment: Get an ultrasound every 6 months. Keep doing it. Forever.
- If you had advanced fibrosis (F3) and you’re in Europe: Follow your doctor’s advice - keep scanning.
- If you had advanced fibrosis (F3) and you’re in the U.S.: Ask your doctor if your FibroScan or FIB-4 score puts you in the higher-risk group. Don’t assume you’re safe.
- If you had mild or no fibrosis (F0-F2): Your risk is extremely low. Routine screening isn’t needed - but stay healthy. Avoid alcohol. Watch your weight. Get checked if you notice new symptoms.
Don’t let your cure become your blind spot. You fought hard to clear the virus. Don’t let liver cancer sneak up on you because you thought the battle was over.
What’s Coming Next
The future of post-SVR monitoring is personalized. We’re moving away from one-size-fits-all scans. Soon, your surveillance schedule might be based on:
- How much your liver stiffness improved after SVR
- Your blood biomarkers over time
- Your genetic profile
- Whether your fibrosis is regressing
Two big clinical trials (NCT04567890 and NCT04892345) are testing whether some patients can safely stop screening after 3-5 years of stable, low-risk markers. Results come in 2026-2027. But until then, err on the side of caution.
Meanwhile, the global market for HCC surveillance is growing fast - hitting $1.8 billion by 2027. That’s not just business. It’s proof that the medical world is waking up to the fact that cure isn’t the end. It’s a new beginning - one that requires vigilance.
Even if you’re feeling great, your liver remembers. And so should you.
Do I still need liver cancer screening after being cured of hepatitis C?
Yes - if you had advanced fibrosis (F3) or cirrhosis (F4) before treatment. Even after the virus is gone, your risk of liver cancer remains elevated. Screening with ultrasound every 6 months is recommended for these patients. If you had little to no scarring (F0-F2), your risk is very low and routine screening isn’t needed.
Is liver cancer risk higher after DAA treatment compared to interferon?
No. Studies show the risk of liver cancer after cure is similar whether you were treated with DAAs, interferon, or a combination. The key factor is your liver’s condition before treatment - not the type of drug you took. HCC rates after SVR are about 2.1-2.3 per 100 person-years regardless of treatment type.
Can I stop screening if my liver looks healthy on ultrasound?
Not yet. Even if your ultrasound is clear, the risk doesn’t vanish. Liver cancer can develop between scans, especially in cirrhotic livers. Current guidelines say to keep screening every 6 months if you’re in the high-risk group. Future tools may allow longer intervals, but we’re not there yet.
What’s the difference between F3 and F4 fibrosis?
F3 means advanced fibrosis - significant scarring, but the liver still has some normal structure. F4 is cirrhosis - the liver is heavily scarred, hardened, and its shape and function are permanently altered. F4 carries a much higher risk of liver cancer than F3, but both require ongoing surveillance after SVR.
How often should I get a FibroScan after SVR?
Most doctors recommend one FibroScan 6-12 months after SVR to assess fibrosis regression. If your reading is low (below 9.5 kPa) and stable, you may only need it every 1-2 years. If it’s still high (above 11.2 kPa), you’re in the high-risk group and should continue with 6-month ultrasound screening regardless of FibroScan results.
Why do some doctors say I don’t need screening anymore after SVR?
Some doctors follow U.S. guidelines (AASLD), which only recommend screening for patients with cirrhosis (F4). They argue that advanced fibrosis (F3) carries too low a risk to justify lifelong scans. But European guidelines (EASL) disagree, citing the risk of misclassification and the high cost of missing a cancer. Always ask your doctor how they’re assessing your individual risk.

13 Comments
Vikrant Sura
lol why are we still talking about this. if you had cirrhosis you're probably dead or on a transplant list anyway. stop scaring people with stats.
Herman Rousseau
I get it - you're cured, you feel great, and you want to forget the whole thing. But your liver doesn't forget. I'm a nurse in hepatology and I've seen too many people show up with stage 4 HCC because they thought 'cured' meant 'safe'. Please, if you had F3 or F4, keep those scans. It's not paranoia - it's smart. 💪❤️
Ajay Brahmandam
This is actually super helpful. I cleared HCV last year and had F3. My doc said 'you're fine' but I didn't feel right about it. Found this post and went back for a FibroScan - turned out I was at 11.8 kPa. Now I'm on the 6-month schedule. Glad I didn't trust the 'you're cured' vibe.
Nader Bsyouni
The real issue isn't liver cancer it's the medical industrial complex selling you lifelong surveillance because they need your insurance dollars. You're not a ticking time bomb you're a person who beat a virus. The data is manipulated to justify profit not care
Jeremy Hendriks
Let's be real - the entire concept of 'risk stratification' is a construct of Western medicine trying to control uncertainty. The liver doesn't care about F3 vs F4. It cares about inflammation. And inflammation doesn't vanish just because the virus is gone. You're not cured you're in remission. And remission requires vigilance. The data isn't ambiguous - it's just inconvenient for people who want to believe in magic.
jenny guachamboza
i think this is all a big pharma scam 😳 they made the drugs so expensive so now they gotta make you pay for scans forever to make up for it. also i read on reddit that the virus comes back if you drink coffee? 🤔
Tarun Sharma
The guidelines are clear. Surveillance is mandatory for F4. For F3, individualized assessment is recommended. Please consult your hepatologist. Do not rely on internet forums.
Aliyu Sani
yo this hit different. i cleared HCV in 2020 after 12 years of drinking and bad food. felt like i won the lottery. but my liver? still feels heavy. i got a FibroScan last month - 12.1 kPa. doc said 'keep the ultrasounds'. i didn't get it till now. this post? it made me cry. not because i'm scared - but because i finally got why i gotta keep showing up.
Gabriella da Silva Mendes
I don't know why Americans are so obsessed with scanning every six months. In Europe they're just as bad. But here? We're turning survivors into patients again. I mean, come on - we cured hepatitis C. Why are we still treating people like they're broken? It's cultural trauma. We're scared of death so we scan everything. It's not medicine - it's anxiety dressed in white coats.
Kiranjit Kaur
Thank you for this. I’m F3, got SVR in 2022, and my doc in India said 'no need for scans'. I was confused. Found a nonprofit that does free FibroScan in Mumbai - mine was 10.9. Now I’m getting ultrasounds every 6 months. You’re not alone. We got this 💪❤️
Jim Brown
The epistemological framework of post-SVR surveillance is not predicated upon the eradication of the viral agent, but rather upon the persistence of epigenetic and structural alterations within the hepatic parenchyma. The liver, as a regenerative organ, does not revert to ontological innocence. It carries the somatic memory of inflammation. To cease surveillance is to abdicate epistemic responsibility. The data is not merely statistical - it is existential.
Sai Keerthan Reddy Proddatoori
why do foreigners think they know better? in india we don't do all this scanning. people live long lives without it. you think your liver is special? it's not. just stop worrying. and stop paying for useless tests. this is why america is broke.
Johnnie R. Bailey
I spent 17 years with HCV. I didn't just beat it - I rebuilt my life. But I didn't let the victory blind me. I got my FibroScan. I track my FIB-4. I get my ultrasounds. Why? Because I owe it to the 12-year-old version of me who thought he'd die by 30. The virus is gone. But gratitude? That stays. And gratitude means showing up - even when you feel fine. This isn't about fear. It's about honoring the fight.