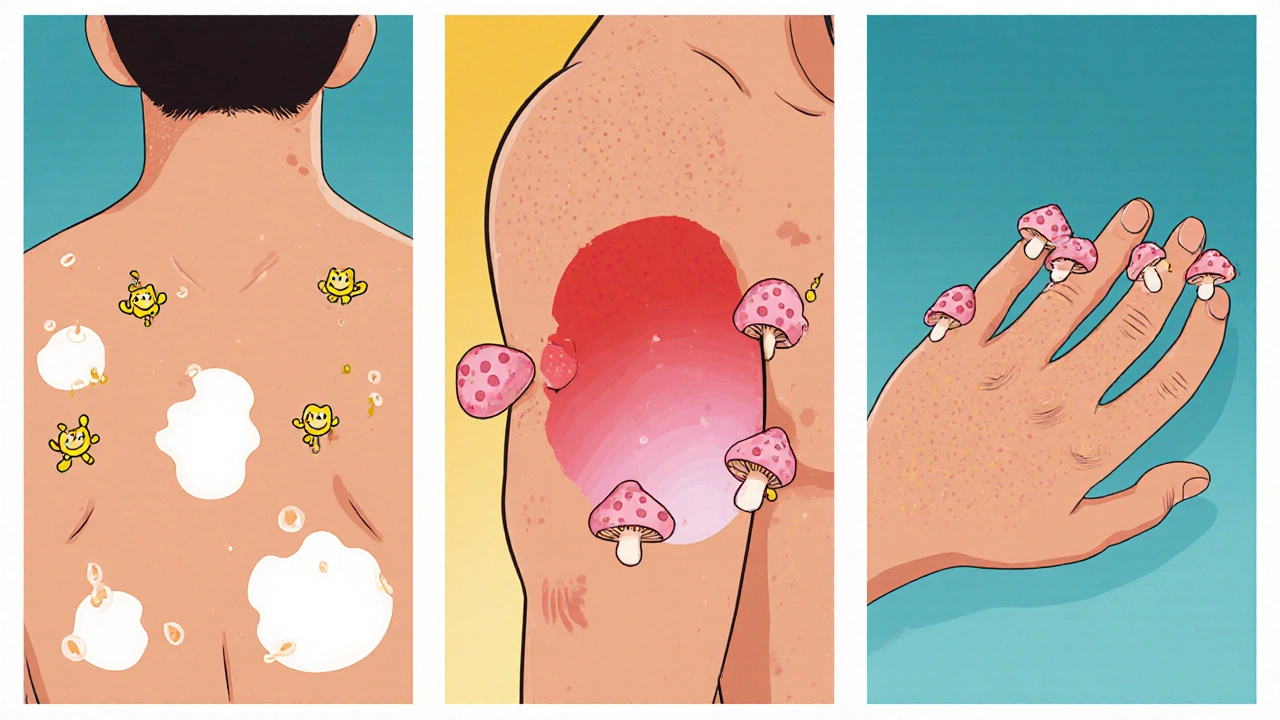
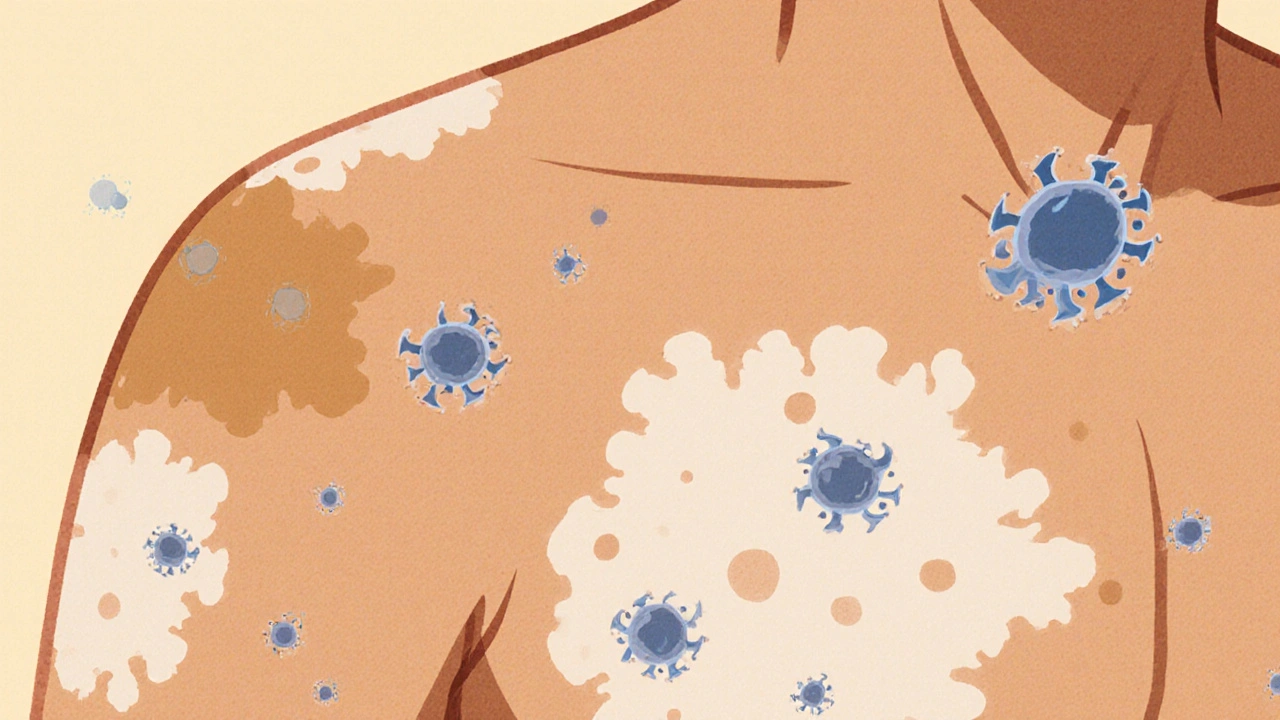
When your skin suddenly develops patches of lighter or darker color, a common culprit is fungal skin discoloration, a condition where certain fungi interfere with the skin’s normal pigment production.
Why Does Skin Change Color?
Skin gets its hue from melanocytes, specialized cells that produce melanin. Anything that disrupts melanin synthesis, destroys melanocytes, or causes inflammation can lead to either hyperpigmentation (darker spots) or hypopigmentation (lighter spots). Fungi can affect pigment in three main ways:
- Direct enzymatic action: Some species release enzymes that break down melanin.
- Inflammatory response: The body’s immune reaction to the infection can damage melanocytes.
- Altered lipid environment: Certain fungi thrive in oily skin, changing the local environment and influencing pigment production.
Understanding these mechanisms helps you spot the early signs before itching or scaling appear.
Common Fungi That Cause Discoloration
Not all fungi affect skin color, but a handful are notorious for it. Below are the three groups you’ll encounter most often.
Tinea versicolor, also known as pityriasis versicolor, is caused by the yeast‑like fungus Malassezia. It typically produces small, irregular patches that range from pale‑white to tan‑brown, especially on the trunk, shoulders, and upper arms. The fungus feeds on skin oils, altering the way melanocytes distribute melanin.
Candida species, especially Candida albicans, are part of the normal skin flora. When they overgrow in warm, moist areas (like skin folds), they can cause red‑to‑pink discoloration that may look lighter in the center and darker at the edges. Unlike Tinea versicolor, Candida often brings a sticky feel and occasional itching.
Dermatophytes such as Trichophyton, Microsporum, and Epidermophyton cause classic ringworm infections. While the primary symptom is a raised, scaly border, some strains produce pigment‑changing lesions, especially on the hands and feet. The discoloration may start light and become darker as the infection persists.
How Fungi Alter Pigment
Each fungal group interferes with pigment in a slightly different fashion.
- Melanin degradation: Malassezia secretes lipases that break down skin lipids, creating a less‑protected environment for melanin. This leads to hypopigmented patches, especially after sun exposure.
- Inflammatory cytokines: Candida triggers a robust immune response, releasing cytokines like IL‑1 and TNF‑α. These chemicals can damage melanocytes, causing irregular dark spots once the infection clears.
- Keratin damage: Dermatophytes digest keratin, the protein that shields melanocytes. As the protective layer thins, melanin either bleaches (lighter spots) or accumulates unevenly (darker spots).
Knowing the pathway helps clinicians decide whether an antifungal alone will reverse the discoloration or if additional skin‑lightening or darkening agents are needed.
Diagnosing Fungal Skin Discoloration
Because the visual signs overlap with other conditions (vitiligo, eczema, post‑inflammatory hyperpigmentation), laboratory confirmation is often required.
KOH test is the go‑to bedside test. A clinician scrapes a tiny skin sample, mixes it with potassium hydroxide, and looks under a microscope. The KOH clears the skin cells, leaving fungal hyphae or yeast spores visible.
Wood's lamp examination uses ultraviolet light. Certain fungi fluoresce-Microsporum glows bright green, while Malassezia shows a yellow‑gold hue. The glow helps differentiate fungal discoloration from other pigment disorders.
In ambiguous cases, a skin culture or a biopsy may be ordered to identify the exact species and guide treatment.
Treatment and Prevention Strategies
Effective therapy targets the fungus and supports the skin’s natural pigment recovery.
- Topical antifungals: Over‑the‑counter creams containing clotrimazole, terbinafine, or ketoconazole work well for mild Tinea versicolor and localized Candida.
- Oral antifungals: For extensive dermatophyte infections or stubborn Candida, a short course of fluconazole or itraconazole may be prescribed.
- Sun protection: Because many fungi exacerbate pigment changes after UV exposure, daily sunscreen (SPF 30+) helps prevent the spots from darkening.
- Hygiene measures: Keep skin dry, change sweaty clothes promptly, and avoid tight, non‑breathable fabrics.
- Adjunct skin care: After the infection clears, gentle exfoliation and moisturizers with niacinamide or vitamin C can even out tone.
fungal skin discoloration often fades within weeks of successful treatment, but persistent spots may need a dermatologist‑approved pigment‑correcting product.

Quick Comparison of Common Culprits
| Fungus | Typical Color Change | Common Body Areas | Preferred Diagnostic Test | First‑line Treatment |
|---|---|---|---|---|
| Malassezia (Tinea versicolor) | Hypopigmented to tan patches | Trunk, shoulders, upper arms | Wood's lamp (gold‑yellow fluorescence) | Topical selenium sulfide or ketoconazole |
| Candida albicans | Red‑pink with possible lighter center | Skin folds, groin, under breasts | KOH test (yeast buds & pseudohyphae) | Topical clotrimazole; oral fluconazole if extensive |
| Dermatophytes (Trichophyton, Microsporum) | Variable; often starts light then darkens | Hands, feet, scalp, nails | KOH test (branching hyphae) | Topical terbinafine; oral itraconazole for deep infections |
Prevention Checklist
- Dry skin thoroughly after showering; pay attention to creases.
- Wear breathable fabrics-cotton or moisture‑wicking sports wear.
- Avoid sharing towels, razors, or shoes.
- Apply antifungal powder or spray in high‑risk areas during hot weather.
- Use a broad‑spectrum sunscreen daily, even on cloudy days.
- Schedule a skin check if discoloration persists longer than 4 weeks after treatment.
Frequently Asked Questions
Can fungal skin discoloration become permanent?
If the infection is treated promptly, most pigment changes fade within a few months. However, prolonged inflammation or repeated infections can cause lasting hyper‑ or hypopigmentation, requiring targeted skin‑brightening or pigment‑darkening therapies.
Is a skin patch that changes color always fungal?
No. Vitiligo, post‑inflammatory hyperpigmentation, and certain bacterial infections can look similar. A KOH test or Wood's lamp exam helps confirm a fungal cause.
Do over‑the‑counter antifungal creams work for all types?
Topical agents are effective for mild Tinea versicolor and localized Candida. Dermatophyte infections that are extensive or involve hair/nails often need oral medication.
Can sunlight make the spots darker?
Yes. UV exposure stimulates melanin production in the unaffected skin, making the lighter patches stand out. Using sunscreen reduces this contrast.
How long does it take for the skin to return to normal after treatment?
Most people see improvement within 2-4 weeks. Full color normalization can take up to 3 months, especially if the infection was deep or the skin was heavily inflamed.

15 Comments
Zachary Blackwell
Ever wonder why the CDC never mentions the real reason behind those weird skin patches? They’ve got a whole agenda to keep us guessing while hidden labs push microbial tech into the populace. The fungi aren’t just opportunistic; they’re engineered vectors in a grand experiment. Keep your eyes open and don’t trust the glossy pamphlets they hand out.
prithi mallick
Life’s little mysteries often hide in the most mundane places – like a sudden speckle on your forearm. It reminds me of how our thoughts can change hue, like the skin itself, when we confront uncertainty. Stay gentle with yourself while navigating these changes; remember, every patch is a story waiting to be understood. Even if the science feels heavy, breathe, and let compassion guide your next step.
We all stumble, and that’s okay.
deepak tanwar
While the article asserts that fungal discoloration is purely a medical issue, one must consider the sociopolitical context in which such information is disseminated. The emphasis on topical creams subtly shifts responsibility onto the individual, diverting attention from systemic environmental factors that facilitate fungal proliferation. Moreover, the omission of socioeconomic disparities in skin health suggests a deliberate narrowing of discourse.
Abhishek Kumar
Meh, same old fungus talk.
hema khatri
Our great nation deserves skin that reflects its strength, not these foreign fungal invaders. It’s infuriating how quickly these pathogens spread when we neglect traditional hygiene practices that our ancestors upheld. Stay vigilant, protect our heritage, and reject the complacency that lets these bugs thrive.
Jennell Vandermolen
I appreciate the thorough breakdown of the different fungi and their mechanisms. It’s helpful to keep a checklist of preventive steps, especially the emphasis on keeping skin dry. If anyone feels overwhelmed, remember that small daily habits can make a big difference over time.
Mike Peuerböck
Excellent synthesis of the pathogenic pathways! The detailed comparison table serves as a valuable reference for clinicians and laypersons alike. By integrating sunscreen use with antifungal therapy, we can mitigate post‑treatment hyperpigmentation. Let’s champion a holistic approach that addresses both microbial eradication and pigment restoration.
Simon Waters
Did you know that some of the “new” fungal strains were first noted in obscure research papers that never made it to mainstream media? It makes you wonder what else they’re keeping under wraps.
Vikas Kumar
Our people have battled skin ailments long before these imported fungi arrived. It’s a testament to our resilience that we can still stand tall against such threats. Let’s prioritize indigenous remedies and community awareness to safeguard our skin.
Shan Reddy
Keeping skin dry and using breathable fabrics can dramatically reduce fungal growth, especially in hot climates. Pair that with a routine of antifungal powder in high‑risk areas, and you’ll notice a marked improvement. Consistency is key; sporadic effort rarely yields lasting results.
Heather ehlschide
From a clinical perspective, distinguishing Malassezia‑induced hypopigmentation from vitiligo can be challenging without proper diagnostic tools. A Wood’s lamp exam offers rapid, non‑invasive differentiation, while a KOH prep confirms fungal presence. Early intervention not only clears the infection but also limits permanent pigment alteration.
Kajal Gupta
The interplay between fungal enzymes and melanin is truly fascinating-like a microscopic tug‑of‑war on our skin’s canvas. When you blend scientific insight with practical prevention tips, the result is both empowering and actionable. Keep sharing such vibrant knowledge!
Michaela Dixon
It’s remarkable how the human body, an ecosystem in its own right, can become a stage for microscopic dramas that play out in visible colors. When Malassezia colonizes oily regions, its lipase activity subtly alters the lipid matrix, which in turn changes how melanin is distributed or protected. This biochemical cascade can manifest as hypopigmented macules that become more pronounced after sun exposure, because the surrounding skin darkens while the affected area remains lighter. Candida, on the other hand, often triggers a robust inflammatory response; the release of interleukins and tumor necrosis factor not only combats the pathogen but also inadvertently damages melanocytes, leading to irregular hyperpigmented borders once the infection recedes. Dermatophytes such as Trichophyton and Microsporum are adept at degrading keratin, the structural scaffold that shields melanocytes. As the keratinous barrier thins, melanin may either clump together or become more exposed, producing a variegated pattern that can evolve over weeks.
Diagnostically, the KOH preparation remains a cornerstone because it quickly clarifies fungal filaments against a background of cleared keratinocytes. Yet, the Wood’s lamp offers a visual cue that can be especially useful in the clinical setting, saving time and resources. The distinct fluorescence of Microsporum (green) versus the golden hue of Malassezia can steer treatment decisions without waiting for culture results. Moreover, the inclusion of a brief patient education segment-emphasizing daily hygiene, prompt drying of skin folds, and the use of antifungal powders-can dramatically lower recurrence rates.
Treatment algorithms should be tiered. For limited Tinea versicolor, topical selenium sulfide or ketoconazole shampoos applied to affected areas for a week often suffice, while more extensive involvement may require oral agents such as itraconazole. Candida infections in moist folds respond well to clotrimazole cream, but when resistant, a short course of fluconazole can eradicate deeper colonization. Dermatophyte infections that involve the nail matrix or extensive body surface often necessitate systemic terbinafine, given its favorable pharmacokinetic profile.
Beyond pharmacotherapy, adjunctive measures can accelerate pigment normalization. Gentle exfoliation with alpha‑hydroxy acids helps remove dead keratinocyte layers that may trap melanin unevenly, while topical vitamin C serums can brighten residual hypopigmented zones by stimulating melanogenesis. Conversely, niacinamide can bolster the skin barrier and reduce post‑inflammatory hyperpigmentation. Of equal importance is the consistent application of broad‑spectrum sunscreen-SPF 30 or higher-to prevent UV‑induced melanocyte overactivity that would otherwise accentuate contrast between affected and unaffected skin.
In summation, fungal skin discoloration is a multifactorial condition where microbiology, immunology, and dermatology intersect. By integrating accurate diagnostics, targeted antifungal regimens, and supportive skin‑care strategies, clinicians can not only resolve the infection but also guide patients toward lasting pigment equilibrium.
Dan Danuts
Wow, that deep dive really ties everything together! I love the practical tips blended with the science-makes it easy to share with friends who might be dealing with those stubborn spots.
Dante Russello
Great job summarizing the whole process! Remember, community support and sharing reliable information are key to preventing these issues. Encourage others to stay consistent with hygiene and follow up with their healthcare providers when needed.