Rheumatoid arthritis isn't just stiff joints or aching hands. It’s your immune system turning on itself-mistaking the lining of your joints for an invader and launching a full-scale attack. This isn’t wear-and-tear arthritis. This is an autoimmune storm that can destroy cartilage, erode bone, and ripple through your lungs, heart, and even your eyes. And while it’s not curable, the way we treat it has changed dramatically in the last 25 years. Today, people with RA aren’t just managing pain-they’re reclaiming their lives.
What Really Happens in Your Joints with RA?
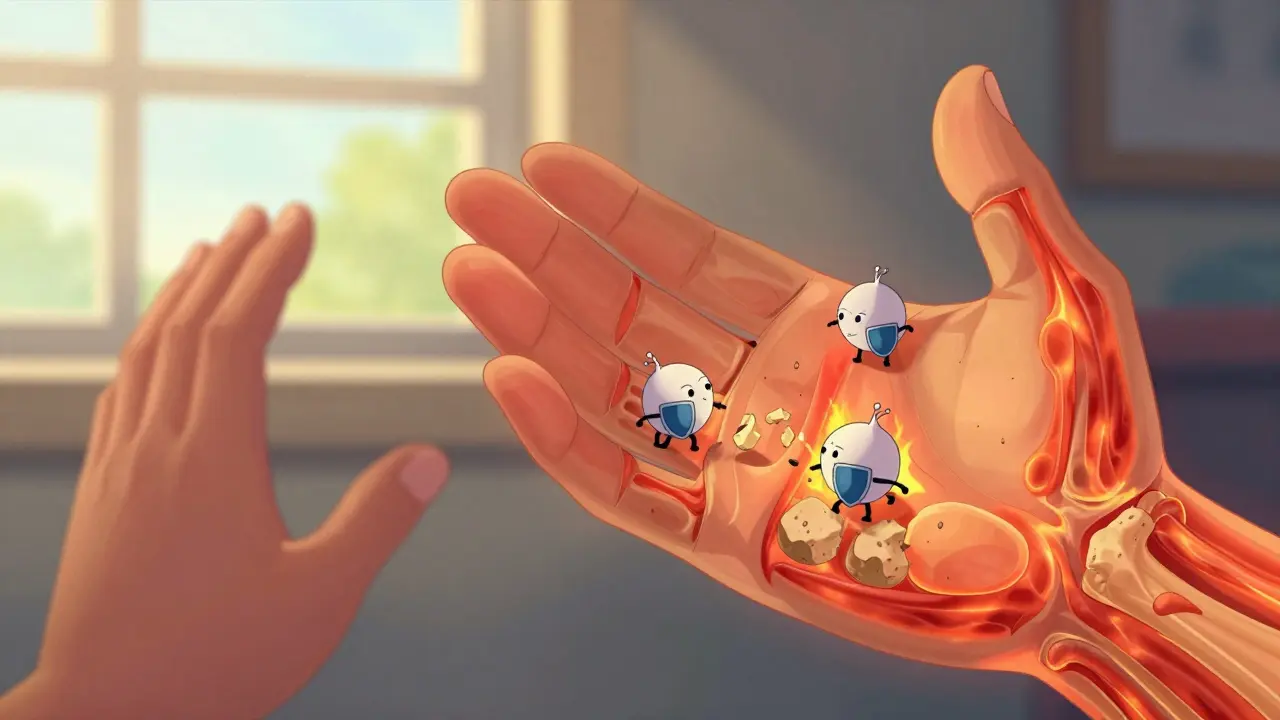
Inside every joint is a thin layer of tissue called the synovium. It’s supposed to make fluid that keeps your joints moving smoothly. In rheumatoid arthritis, your immune system sends white blood cells and antibodies straight to that lining. They don’t just cause swelling-they start eating away at it. Over time, the synovium thickens, becomes inflamed, and starts destroying the cartilage and bone around it. That’s why RA doesn’t just hurt-it deforms.
Unlike osteoarthritis, which shows up in one knee from years of running or lifting, RA is symmetrical. If your left wrist is swollen, your right one will be too. It often starts quietly-in the small joints of your fingers and toes-before spreading to wrists, knees, and ankles. Morning stiffness isn’t just annoying; it’s a key sign. If you can’t move your fingers for 45 minutes or longer after waking up, that’s not normal aging. That’s RA.
And it’s not just joints. About 1 in 10 people with RA develop Sjögren’s syndrome-dry eyes, dry mouth, constant discomfort. Others get rheumatoid nodules-hard lumps under the skin near elbows or heels. Some face lung scarring, anemia, or a doubled risk of heart disease. RA doesn’t stay in the joints. It’s a whole-body disease.
How Is RA Diagnosed?
There’s no single test for RA. Doctors piece it together like a puzzle. Blood tests look for rheumatoid factor (RF) and anti-CCP antibodies-markers that show your immune system is attacking your own tissue. But not everyone with RA tests positive. That’s why symptoms matter just as much.
Physical exams check for warmth, swelling, and reduced range of motion. X-rays and ultrasounds show early signs: soft tissue swelling, then bone thinning around joints, and eventually, tiny holes where bone has been eaten away. If you’ve had pain and swelling in multiple joints for six weeks or more, especially with morning stiffness lasting over 30 minutes, that’s a red flag.
Early diagnosis is everything. The first 3 to 6 months after symptoms start are the window where you can stop damage before it’s permanent. Delay treatment, and you risk irreversible joint destruction. That’s why specialists push so hard for quick referrals to rheumatologists.
First-Line Treatment: Methotrexate and Why It Still Matters
Before biologics, methotrexate was the only real weapon against RA. Today, it’s still the first step for nearly 7 out of 10 new patients. It’s cheap, effective, and has been used for decades. It doesn’t cure RA, but it slows the immune system’s attack enough to reduce swelling, pain, and joint damage.
But it’s not magic. About 40% of people don’t respond well enough to methotrexate alone. Others can’t tolerate the side effects-nausea, fatigue, liver stress. That’s where things change. When methotrexate isn’t enough, doctors turn to biologics.
Biologic Therapies: Targeting the Immune System’s Attackers
Biologics are different from older drugs. Instead of broadly suppressing the immune system, they zero in on specific troublemakers-like a sniper instead of a bomb. They’re made from living cells, not chemicals, and are given by injection or IV.
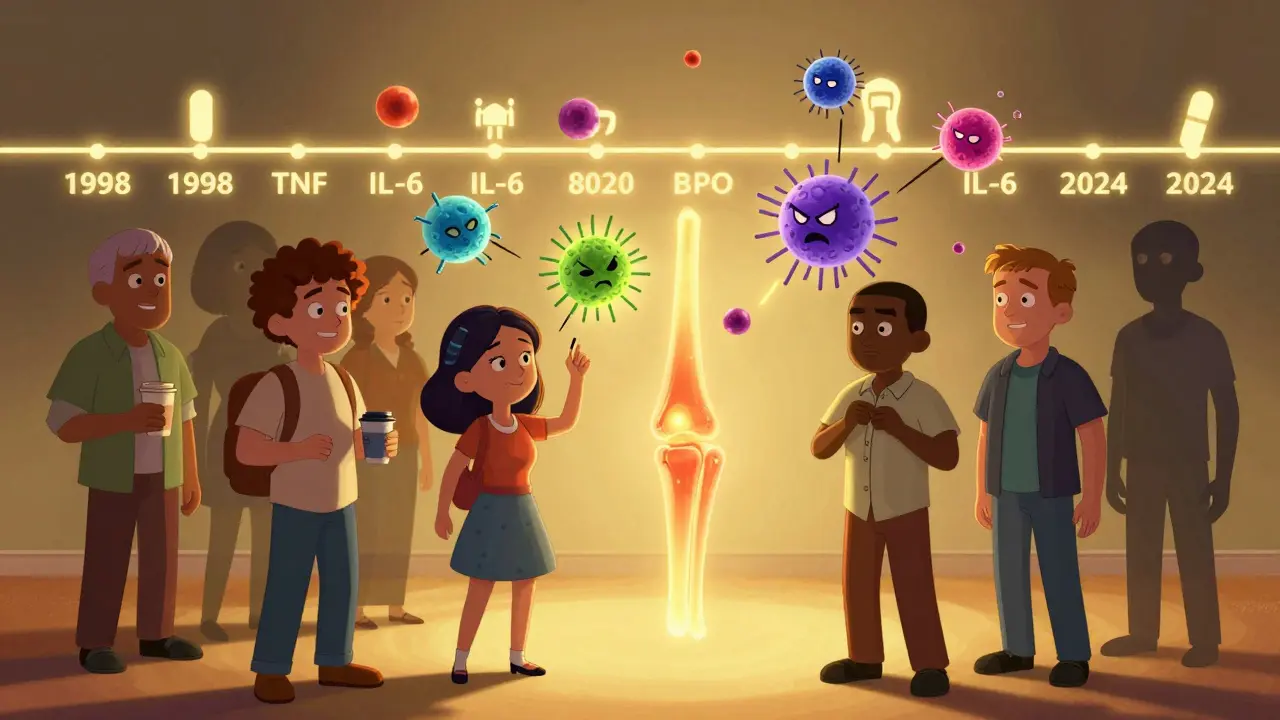
Here’s what’s out there:
- TNF inhibitors (adalimumab, etanercept, infliximab): Block tumor necrosis factor, a major driver of inflammation. These were the first biologics approved in 1998 and still make up over half of all biologic prescriptions.
- IL-6 inhibitors (tocilizumab): Target interleukin-6, a protein linked to joint damage and fatigue. Used for patients who don’t respond to TNF blockers.
- B-cell inhibitors (rituximab): Deplete B-cells, the immune cells that produce harmful antibodies. Often used after other biologics fail.
- T-cell blockers (abatacept): Stop T-cells from activating other immune cells. A good option for people with high infection risk.
Studies show that when biologics are combined with methotrexate, about 60% of patients cut their disease activity in half or more. Without methotrexate, the success rate drops. That’s why they’re almost always used together.
Real people report real results. Sarah, 42, couldn’t play piano for five years because her fingers were locked in pain. After starting tocilizumab in 2022, she played again. On patient forums, people talk about buttoning shirts, carrying groceries, and sleeping through the night-things they hadn’t done in years.
The Cost and Risk of Biologics
Biologics aren’t cheap. Annual costs range from $15,000 to $60,000. Even with insurance, out-of-pocket expenses can hit $5,000 a year. That’s why nearly half of patients struggle to stay on treatment. Some skip doses. Others stop entirely.
And there’s a trade-off. Because biologics weaken parts of your immune system, you’re more vulnerable to infections. The risk of serious infections like pneumonia or tuberculosis is 1.5 to 2 times higher than with methotrexate alone. That’s why doctors test for TB before starting treatment and advise against biologics if you’ve had recent infections or hepatitis.
There’s also a small but real increase in lymphoma risk. It’s rare-about 1 in 1,000 patients-but it’s why the FDA requires special safety programs for all biologics. You need to know the signs: unexplained fever, night sweats, swollen lymph nodes.
And then there’s the emotional toll. Managing RA isn’t just about pills and shots. It’s about fear-fear of flares, fear of disability, fear of being a burden. Many patients feel isolated. That’s why support groups and apps like MyRA matter. They’re not just tools-they’re lifelines.

What’s New in RA Treatment?
The field is moving fast. In 2023, the first biosimilar to adalimumab (Humira) got FDA approval. Biosimilars are nearly identical to the original drug but cost 15-20% less. That’s huge for patients and the system. By 2027, they could save billions.
New drugs are coming too. Upadacitinib (Rinvoq), a JAK inhibitor, got expanded approval for early RA in early 2024. It works differently from biologics-taken as a pill instead of an injection-and shows strong results in patients who didn’t respond to TNF blockers.
Even more exciting are the drugs in late-stage trials. Deucravacitinib, a TYK2 inhibitor, targets inflammation at a deeper level with fewer infection risks. Early data looks promising. Researchers are also working on blood tests that can predict who will respond to methotrexate or biologics before they even start treatment. One study in 2023 used genetic markers to predict response with 85% accuracy.
Living With RA: Beyond Medication
Medicine is only half the battle. Exercise isn’t optional-it’s medicine. The CDC recommends 150 minutes of moderate activity a week. Walking, swimming, cycling-anything that keeps your joints moving without pounding them. Studies show people who stay active have less pain and slower joint damage.
Weight matters too. Losing just 5-10% of your body weight can reduce RA symptoms by 20-30%. That’s not because fat is “bad”-it’s because fat tissue produces inflammatory chemicals. Less fat means less inflammation.
And don’t underestimate rest. RA flares aren’t just physical-they’re exhausting. Learning when to push and when to pause is a skill. Many patients use apps to track symptoms, medication side effects, and sleep patterns. That data helps doctors adjust treatment faster.
Support networks help. The Arthritis Foundation’s Live Yes! program connects over 100,000 people annually. CDC workshops teach self-management skills that cut pain by 20% in six months. You’re not alone. And you don’t have to do this alone.
What’s Next for RA?
The goal isn’t just to reduce pain. It’s to reach remission-no swelling, no fatigue, no damage. And it’s possible. With early treatment and the right combo of drugs, up to 40% of patients can achieve this by 2030, according to projections from the Arthritis Foundation.
But disparities remain. Rural patients are 30% less likely to get biologics. Access to rheumatologists is still limited. Insurance hurdles delay treatment. These aren’t just medical problems-they’re systemic ones.
What’s clear is this: RA doesn’t have to mean a life of pain. The tools are here. The science is advanced. The challenge now is making sure everyone who needs treatment can get it-not just those who can afford it or live near a big hospital.
If you’ve been told your joint pain is just aging, get a second opinion. If you’ve been struggling with stiffness that lasts for hours, talk to a rheumatologist. You don’t have to live like this. There’s a better way-and it’s available now.


15 Comments
Matt Davies
Man, this post hit different. I’ve seen friends go from barely holding a coffee cup to playing guitar again after starting biologics. It’s not just medicine-it’s magic with a syringe. The fact that someone can get their life back after years of pain? That’s the real win.
Monte Pareek
Let me tell you something real-RA doesn’t care if you’re rich, poor, or in between. I’ve worked in rural clinics for 12 years. Half the people who need biologics can’t get them because the nearest rheumatologist is 200 miles away and insurance won’t cover the trip. We’re talking about people skipping doses because they can’t afford the co-pay. This isn’t just a medical issue-it’s a justice issue. We need better access, not just better drugs.
mary lizardo
While the article presents a compelling narrative, it conspicuously omits the fact that biologics are often prescribed without adequate consideration of long-term immunological consequences. The pharmaceutical industry’s influence on clinical guidelines is neither transparent nor ethically neutral. One must question whether this is medicine-or marketing masquerading as science.
jessica .
biologics are just a cover-up for the government’s secret vaccine agenda. they’re not treating RA-they’re weakening your immune system so you’re easier to control. and why are all these drugs made by big pharma in switzerland? who’s really behind this? you think they care if you live or die? they just want your data and your money.
Ryan van Leent
why do people think this stuff works anyway i mean look at all the side effects nobody talks about the real cost its not just money its your whole life you become a walking pharmacy and for what a few less aches
Isabel Rábago
It’s not just about joints. It’s about dignity. When you can’t hold your child because your hands are fused, you don’t need a drug-you need a miracle. And yet, here we are, talking about biosimilars and JAK inhibitors like it’s a tech launch. People are suffering in silence because they’re told to ‘just be patient.’ Patience is not a treatment.
Anna Sedervay
One cannot help but observe the conspicuous absence of any mention of the systemic corruption within the rheumatology industry. The FDA's safety protocols are performative, and the so-called 'remission' metrics are statistically manipulated to appease investors. The real victory lies not in suppressing inflammation-but in exposing the profit-driven architecture that commodifies chronic pain.
Ashley Bliss
Think about it-your body turns against you. Not because you did something wrong. Not because you’re weak. But because the universe, in its infinite cruelty, decided to make your immune system a traitor. And then we put you on a $60,000-a-year drug to fix it. That’s not medicine. That’s a cosmic joke with a co-pay. And the worst part? You’re still alone in the dark, even when you’re ‘doing better.’
holly Sinclair
What fascinates me is the philosophical paradox embedded in RA treatment: we are using highly targeted biological agents to suppress a system that, in its malfunction, is trying to protect us. So we are essentially punishing the very mechanism that evolved to keep us alive. Is this healing-or is it a form of self-betrayal? If our immune system is mistaken in its attack, does that mean the body is not the enemy, but the messenger? And if so, what is it trying to tell us about our environment, our diet, our stress levels? We treat the symptom, but we refuse to interrogate the cause. That’s not science. That’s avoidance dressed in white coats.
Allison Pannabekcer
I just want to say to anyone reading this who feels alone-you’re not. I’ve had RA for 18 years. Some days are brutal. Some meds didn’t work. Some doctors didn’t listen. But I found a community online, started swimming twice a week, and learned to say ‘no’ without guilt. You don’t have to ‘beat’ RA. You just have to live with it in a way that still lets you breathe. You’re allowed to have bad days. You’re allowed to need help. You’re allowed to still be you.
Sarah McQuillan
actually osteoarthritis is way worse because at least with ra you get all these fancy drugs and people feel bad for you but with oa you just get told to lose weight and take tylenol like its your fault you got old i mean come on
Aboobakar Muhammedali
i read this in my village in india where no one knows what ra is. my cousin has swollen hands and we think its dust or bad water. this post made me cry. thank you for writing this. i will translate it. someone here needs to know
Mark Able
you know what’s wild? the fact that people still think methotrexate is the gold standard. it’s literally a chemo drug repurposed as a bandaid. we’re treating an autoimmune disease with something that was designed to kill cancer cells. we need to stop patching and start rewiring
Chris Clark
my uncle got on a biologic and now he hikes every weekend. used to sit in a chair and cry because he couldn’t open a jar. now he makes his own pickles. i swear this stuff is like turning back time. if you’re scared of the cost or side effects-talk to someone who’s been there. it’s not perfect but it’s worth it
Danielle Stewart
Just wanted to say thank you for writing this. My mom’s been on a JAK inhibitor for a year now-she’s sleeping through the night for the first time in 12 years. It’s not a cure, but it’s a gift. Keep sharing stories like this. They matter more than you know.