When you’re on a trip and notice an itchy, red patch on your skin, you might be dealing with a Skin Yeast Infection, a common fungal infection of the skin caused primarily by the yeast Candida albicans, characterized by redness, itching, and sometimes a flaky rash. It thrives in warm, moist environments - exactly what travel can unintentionally create.
What Exactly Is a Skin Yeast Infection?
A Skin Yeast Infection typically involves the overgrowth of Candida Albicans. While most people carry this yeast harmlessly on their skin and mucous membranes, factors like heat, sweat, and friction can tip the balance, allowing the organism to multiply.
Typical signs include:
- Redness that may spread outward
- Intense itching or burning
- Small, raised bumps that can ooze
- Flaky or cracked skin, especially in folds
Why Traveling Can Trigger or Worsen an Outbreak
Travel introduces three main challenges for anyone prone to fungal growth:
- Temperature and humidity spikes - crowded buses, tropical destinations, and night‑time sweating create the perfect breeding ground.
- Limited access to clean, dry clothing - quick changes, laundry delays, and shared facilities mean skin stays damp longer.
- Stress and altered immune response - jet lag, altered sleep, and the stress of new surroundings can temporarily lower immune defenses, giving the yeast a foothold.
Spotting the Symptoms Early While on the Road
Because you’re often on the move, a subtle rash can go unnoticed until it flares. Keep an eye on these tell‑tale signs:
- Itching that gets worse after a sweaty activity (e.g., hiking, dancing).
- A rash that appears in warm, hidden spots - under the bra strap, between toes, or in the groin.
- Skin that looks shiny or ‘wet’ rather than dry.
If you catch it early, treatment is faster and you’re less likely to miss any travel plans.
Prevention Checklist for the Savvy Traveler
Think of these as your travel‑ready armor against fungal flare‑ups. Most items fit easily in a day‑pack.
- Moisture‑Wicking Clothing - fabrics that pull sweat away from the skin keep the environment dry.
- Powder or antifungal spray for feet and skin folds - apply after showering.
- Quick‑dry socks made of merino wool or synthetic blends - they stay breathable even when damp.
- Carry a small Antifungal Cream (clotrimazole 1% or miconazole 2%). Apply at the first sign of irritation.
- Practice Footwear Hygiene: alternate shoes daily, let them air out, and use a UV shoe sanitizer if possible.
- Include a daily Probiotic Supplement (e.g., Lactobacillus rhamnosus) to support gut health, which indirectly helps skin balance.
- Stay hydrated - drinking water helps maintain healthy skin turnover.
- Limit time in hot tubs, saunas, and public pools where yeast can linger.
Treatment Options When an Outbreak Happens Abroad
Not all treatments are equal, especially when you’re far from a pharmacy. Below is a quick comparison to help you decide what to carry.
| Option | How It Works | Typical Duration | Travel Suitability |
|---|---|---|---|
| Antifungal Cream | Directly kills yeast on the skin surface | 5‑7 days | Very portable; no prescription needed in most countries |
| Oral Antifungal Medication | Systemic treatment that reaches deeper skin layers | 7‑14 days | Requires prescription; keep a copy of the prescription handy |
| Natural Remedies (tea tree oil, yogurt masks) | Antimicrobial properties; may restore skin flora | Varies; usually 10+ days | Easy to pack, but effectiveness less predictable |
If you’re unsure which route to take, start with a topical antifungal cream. If the rash spreads beyond a few centimeters or persists after a week, seek oral therapy from a local doctor.
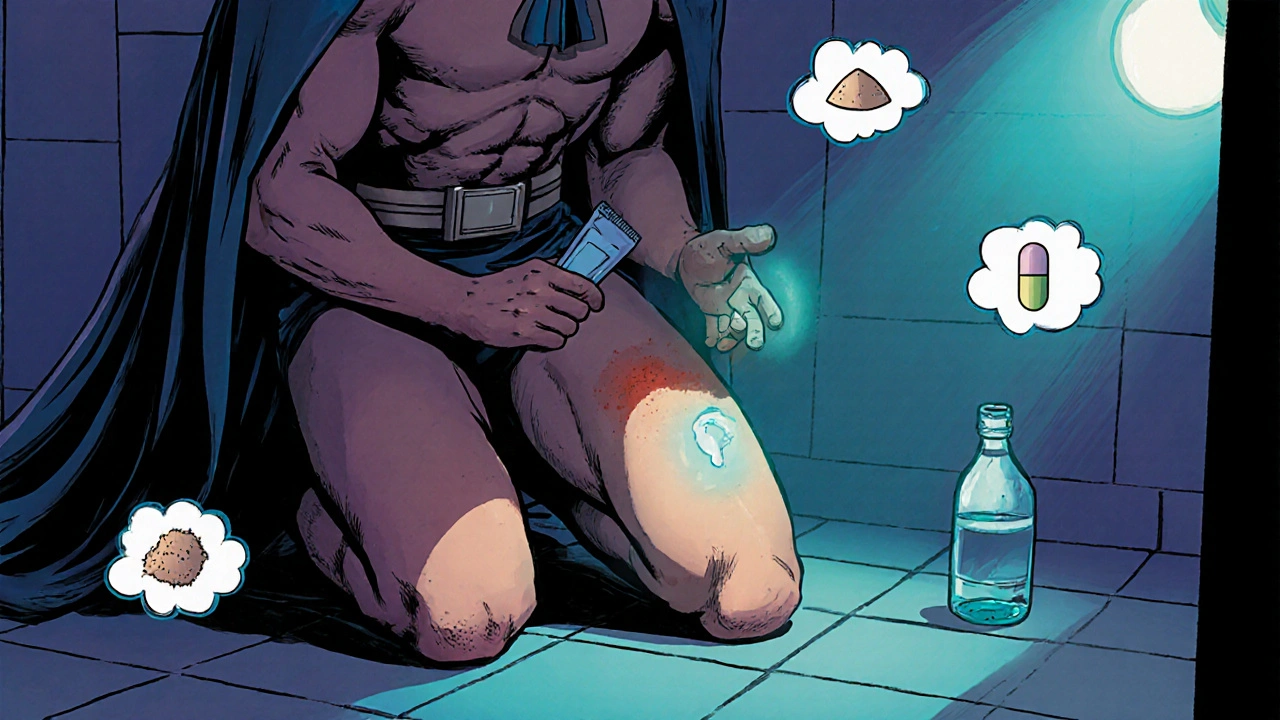
Managing a Flare‑Up on the Road
Here’s a step‑by‑step plan you can follow anywhere from a hostel bathroom to an airport lounge:
- Clean the area with mild soap and lukewarm water. Pat dry - never rub.
- Apply a thin layer of Antifungal Cream twice daily.
- Cover with a breathable, non‑cotton dressing if the area is prone to friction.
- Take a probiotic supplement to help rebalance your gut flora.
- Stay hydrated and avoid sugary drinks, which can feed yeast.
- If there’s no improvement after 72hours, locate a pharmacy or clinic, show your prescription (or request a tele‑medicine consult), and consider an oral dose.
Remember, most airlines and many travel insurance policies cover short‑term medical visits for skin conditions, so keep your policy details handy.
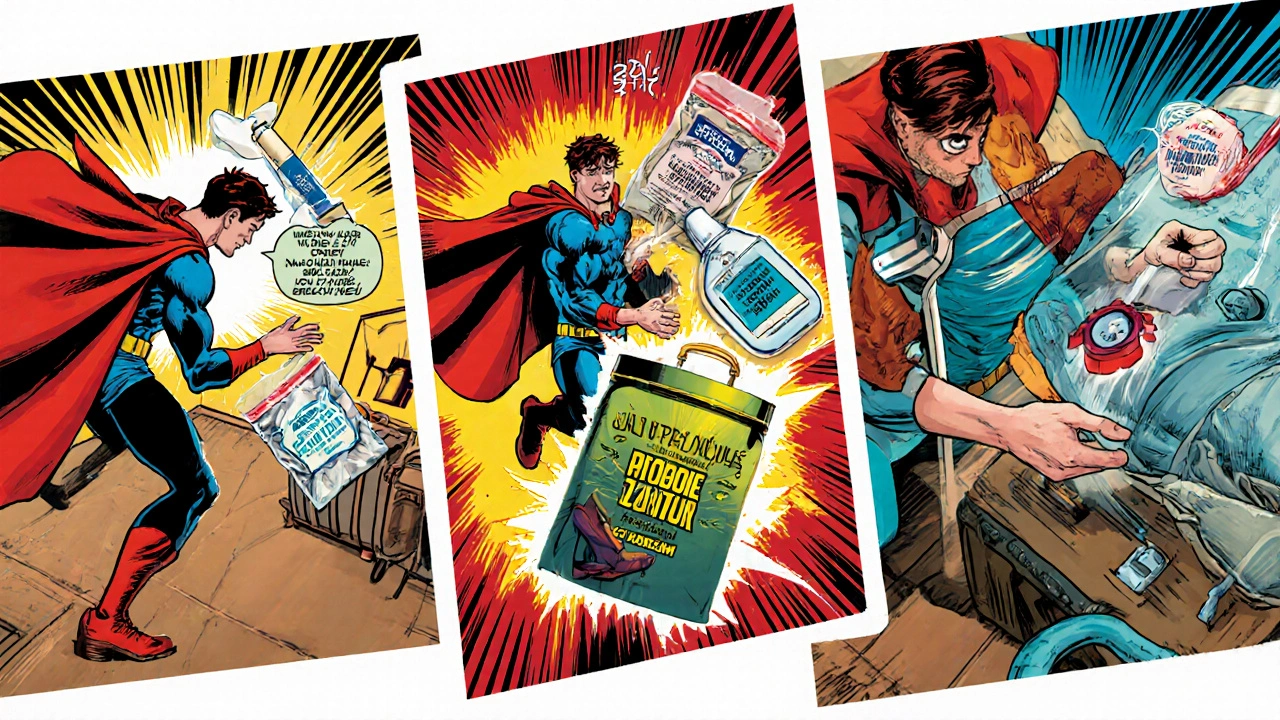
Essential Items for a Yeast‑Safe Travel Kit
Pack these items in a zip‑lock pouch - they’re lightweight and won’t trigger luggage alarms.
- Small tube of Clotrimazole 1% Cream (15g)
- Travel‑size antifungal powder (e.g., miconazole powder)
- Two pairs of moisture‑wicking underwear
- Compact probiotic capsules (30‑day supply)
- Reusable silicone sweat‑absorbing pads for body folds
- UV shoe sanitizer or a small bottle of disinfecting spray
All these items fit into a standard toiletry bag, leaving room for your passport and camera.
When to Seek Professional Help
Most mild outbreaks resolve with self‑care, but see a doctor if you notice any of the following:
- Rapid spreading beyond a few centimeters
- Severe pain, swelling, or pus
- Fever or chills (signs of secondary infection)
- Recurring episodes despite regular prevention
International travel clinics often have English‑speaking staff and can prescribe oral antifungals on the spot.
Quick Recap: Your On‑The‑Go Yeast‑Defense Plan
- Know the symptoms and check daily, especially after sweaty activities.
- Stay dry: wear moisture‑wicking fabrics, change quickly, and powder skin folds.
- Carry a small tube of antifungal cream and a probiotic supplement.
- Use the treatment table to decide between topical, oral, or natural options.
- Don’t hesitate to see a local clinician if the rash worsens.
Frequently Asked Questions
Can I get a skin yeast infection from a hotel bed?
Direct transmission from beds is rare. The infection usually comes from your own skin flora taking advantage of warm, moist conditions. However, shared towels or clothing can spread the yeast, so use your own clean linens when possible.
Is it safe to use over‑the‑counter antifungal cream on sensitive areas?
Yes, most OTC creams (clotrimazole, miconazole) are formulated for sensitive skin. Apply a thin layer and avoid using on broken skin unless a doctor advises otherwise.
How long should I keep a treatment course going after symptoms disappear?
Continue the cream for at least 48hours after the rash clears. This helps eliminate any lingering yeast and reduces recurrence risk.
Do probiotics really help prevent skin yeast infections?
Research shows that certain strains (e.g., Lactobacillus rhamnosus) can improve gut flora, which in turn supports skin health. While not a cure, daily probiotics are a low‑risk preventive measure, especially during travel stress.
Can I use natural remedies like tea tree oil instead of prescription meds?
Tea tree oil has antifungal properties, but concentration matters. A 5% dilution can help mild cases, yet severe or widespread infections usually need medical‑grade antifungals.


11 Comments
Yassin Hammachi
Traveling bumps into our skin’s tiny ecosystems, and when moisture meets Candida, it’s like setting a tiny campfire that can flare up on a hiking trail. Keeping the skin dry, especially in folds, is the simplest armor you can wear. Moisture‑wicking fabrics do more than keep you comfortable; they actually starve the yeast of its favorite habitat. Changing out of sweaty clothes quickly and patting the skin dry can make the difference between a quick itch and a full‑blown rash. Even a tiny towel in your pack for a quick swipe can be a game‑changer. Probiotics aren’t a miracle cure, but they help maintain a balanced gut‑skin axis, which indirectly keeps the fungal overgrowth in check. And don’t forget those little silicone pads – they’re cheap, reusable, and keep those hidden creases from staying damp. A little forethought means you spend more time seeing sights and less time dealing with a dermatologist abroad. Stay curious, stay dry, and enjoy the journey.
Michael Wall
People need to stop treating travel like an excuse to live in a sweaty sauna. If you can’t manage a couple of extra underwear or a quick change, you’re basically inviting fungus to set up camp on you. Simple hygiene isn’t optional; it’s a responsibility. Pack that powder and actually use it – don’t just stare at it in your bag hoping it’ll work by magic.
Christopher Xompero
Okay, listen up, fam! I just walked into a hostel, slipped on my brand‑new merino socks, and BAM! The itch hit me like a plot twist in a bad soap opera. I swear the yeast was throwing a party on my ankle, and nobody was invited!
Pro tip: if you’re not spraying that anti‑fungal spray after every shower, you might as well hand the yeasty invaders a VIP pass. And yeah, the travel‑size cream? It’s like the superhero cape of the skin‑care world – wear it and save the day. Don't be that guy who thinks "I'll just wait it out" – you’ll end up looking like a rash‑ridden zombie on the next tour bus. Trust me, I’ve lived it.
Irene Harty
It is imperative to acknowledge that certain commercial moisturizers contain hidden sterols that can inadvertently nourish Candida colonies. While the guide rightly emphasizes dryness, one must also scrutinize the excipients in publicly provided toiletries to avoid covert cultivation of fungal agents. A cautious approach includes requesting hypoallergenic, preservative‑free soap alternatives when staying in communal accommodations.
Jason Lancer
Just skip the powder and suffer the itch.
Brooks Gregoria
Honestly, the whole panic over skin yeast is blown out of proportion. You’re not walking around with a zombie apocalypse on your thighs – it’s a harmless organism that’s only a problem because we let it. If you’re constantly fearing it, you’re giving it power. Lighten up, wear breathable fabrics, and stop treating every little itch like the end of the world.
Sumit(Sirin) Vadaviya
Traveling with a tiny fungal foe can feel daunting, but a well‑packed kit makes it manageable 😊. Make sure your antifungal cream is in a zip‑lock bag to keep it from melting, and remember to re‑apply after any sweaty activity. A quick spray of antifungal powder on feet and skin folds after a shower can vastly reduce moisture buildup. Even on long flights, a small wipe‑down with a mild, fragrance‑free cleanser helps keep the skin barrier intact. Stay proactive, stay dry, and the yeast won’t get a chance to set up camp.
lindsey tran
okay, so i get it-yeast is stuff that loves wimpy sweaty spots-but you don' gotta be a total drama queen about it. just grab some fun socks and powdeer and *voila* you’re good! i moved my whole pack into a tiny bag and still had space for a tube of clotrimazle… that’s like, magic. remember, dont let a lil itcha ruin ur whole vacay, lol!
Krishna Sirdar
Hey folks, just a friendly reminder that a little mindfulness goes a long way. Check your skin each night, especially after a long hike or a dance night. If you notice any redness, dry it gently and pop on some powder. It’s a small habit that can stop a bigger problem. Stay kind to your skin, and it’ll take care of you while you explore the world.
becca skyy
Cool tip from the guide: quick‑dry socks are a game changer. I’ve tried a few brands and the merino blend really does wick away sweat. Also, the UV shoe sanitizer might sound fancy, but it actually kills a lot of the microbes that travel with you. Just pop your shoes in for a few minutes and you’re good to go. Small steps, big comfort.
Theo Roussel
From a dermatological formulation standpoint, clotrimazole’s mechanism of action involves inhibition of lanosterol 14α‑demethylase, thereby disrupting ergosterol synthesis in fungal cell membranes. This pharmacodynamic profile makes it particularly effective for localized Candida overgrowth, especially when applied twice daily as per the protocol outlined. Ensure the affected area is dry to maximize the drug’s bioavailability.