When a drug has a narrow therapeutic index (NTI), even tiny changes in how it’s absorbed by the body can mean the difference between healing and harm. Think of it like walking a tightrope-too little, and the drug doesn’t work; too much, and it becomes toxic. That’s why generic versions of NTI drugs like warfarin, phenytoin, digoxin, and levothyroxine can’t be approved the same way as regular generics. They need something called a bridging study-a more rigorous, highly controlled test to prove they’re just as safe and effective as the brand-name version.
Why NTI Drugs Are Different
Not all drugs are created equal. Most medications have a wide safety margin. You can take a little more or a little less, and your body handles it. But NTI drugs don’t play that way. Their therapeutic dose is dangerously close to their toxic dose. The FDA defines an NTI drug as one where the ratio between the minimum effective dose and the minimum toxic dose is 2:1 or less. That means if you’re prescribed 5 mg to control your seizures or thin your blood, 6 mg could land you in the hospital.
These drugs also require regular blood monitoring. Doctors check levels to make sure you’re in the sweet spot. Even a 10% shift in how your body absorbs the drug can throw that balance off. That’s why a generic version of warfarin that’s 15% less bioavailable might not just be less effective-it could cause a clot. And one that’s 15% more? It could cause a bleed.
That’s the core problem bridging studies solve. They don’t just ask: ‘Is this generic close enough?’ They ask: ‘Is this generic safe enough?’
How Bridging Studies Work for NTI Generics
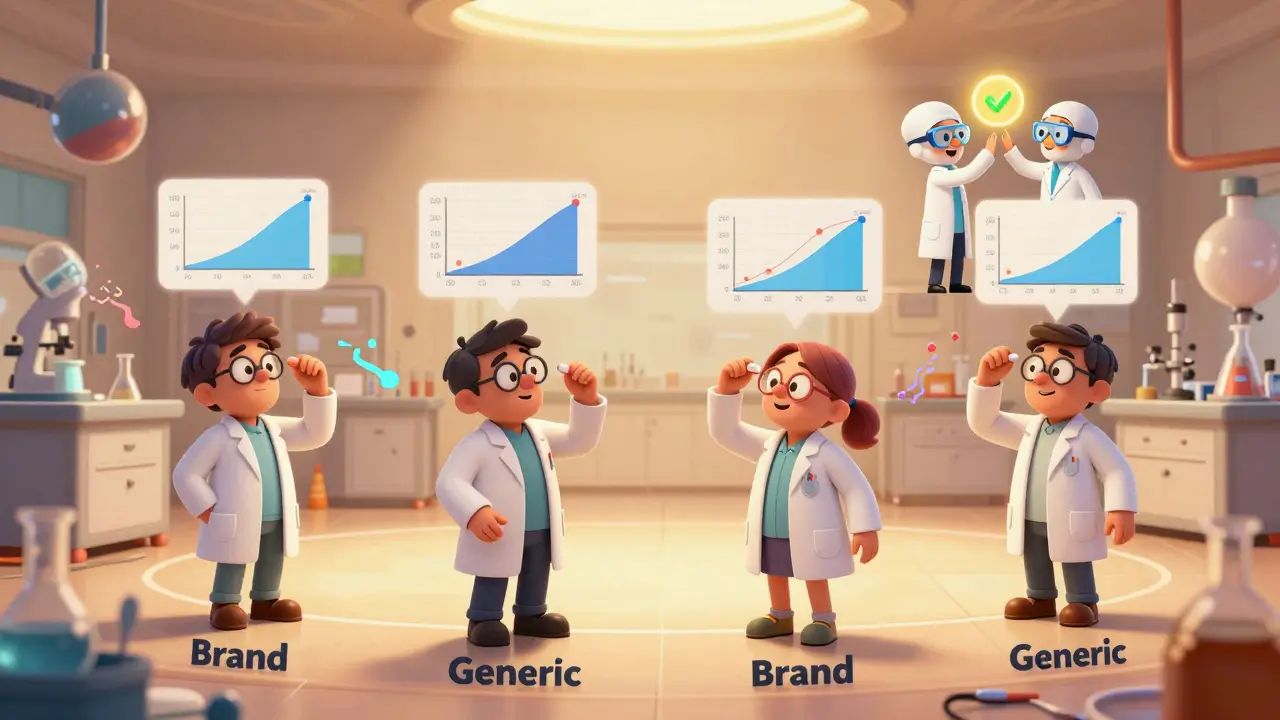
For regular generics, bioequivalence is usually proven with a simple two-way crossover study in healthy volunteers. You take the brand drug once, the generic another time, and compare blood levels. Acceptance? If the generic’s absorption falls between 80% and 125% of the brand, you’re good to go.
For NTI generics? That’s not enough.
The FDA requires a four-way, fully replicated crossover design. That means each participant takes the brand drug twice and the generic drug twice, over several weeks. Why? To account for variability-not just between people, but within the same person. Some NTI drugs behave differently in the same person from one day to the next. The four-way design captures that.
The acceptance criteria are tighter too. Instead of 80-125%, the 90% confidence interval for the geometric mean ratio of Cmax (peak concentration) and AUC (total exposure) must fall between 90.00% and 111.11%. That’s a much narrower window. And the assay limits? They’re tightened to 95-105% for drug content, versus 90-110% for non-NTI drugs.
This isn’t just theory. It’s based on real-world data. Studies on warfarin showed that even small differences in bioavailability led to measurable changes in INR levels-something doctors track closely to prevent strokes or bleeding. The FDA’s 2017 guidance on warfarin tablets was a turning point. It set the standard for how all NTI generics must be tested.
Cost, Time, and Complexity
Developing an NTI generic isn’t just harder-it’s exponentially more expensive and time-consuming.
A standard bioequivalence study costs between $1.5 million and $2.5 million. For an NTI generic? That jumps to $2.5 million to $3.5 million. Why? The four-way crossover needs twice as many participants. Each subject spends 12 to 18 months in the study, with multiple clinic visits, blood draws, and washout periods. Dropout rates are higher. One participant leaves, and you might have to start over with a new group.
It also takes longer. A standard generic can be developed in 2-3 years. An NTI generic? 3-5 years. And even then, the FDA rejects nearly 4 out of 10 applications-not because the drug doesn’t work, but because the bridging study design didn’t meet the standard. In 2022, 37% of complete response letters for NTI generics cited inadequate study design as the main issue. For non-NTI generics? Only 12%.
And not every company is equipped to handle it. Only about 35% of generic manufacturers have the in-house pharmacokinetic modeling and statistical expertise needed to design and analyze these studies. Many have to hire consultants or partner with specialized CROs, adding even more cost and delay.
Why Market Penetration Is So Low
Despite NTI drugs making up about 14% of all small-molecule medications, they account for less than 6% of generic approvals between 2018 and 2022. The result? Only 42% of the NTI drug market is covered by generics-compared to 85% for non-NTI drugs.
That’s not because manufacturers don’t want to enter the market. It’s because the barriers are so high. When a company spends $3 million and five years to develop a generic version of levothyroxine, only to face a 37% rejection rate, they start asking: Is this worth it?
And the payoff isn’t always clear. Even when approved, some prescribers and patients remain skeptical. A doctor who’s seen a patient stabilize on a brand-name drug may hesitate to switch-even if the generic is approved. That’s why education and transparency matter. Clear labeling, consistent manufacturing, and real-world outcome data are slowly building trust.
Regulatory Differences Around the World
The FDA leads the way with its strict NTI guidelines, but other agencies are catching up. The European Medicines Agency (EMA) doesn’t have a formal list of NTI drugs, but its Committee for Medicinal Products for Human Use (CHMP) has made it clear: NTI drugs require special study designs, and those can’t be waived based on similarity alone.
There’s a push for global harmonization through the International Council for Harmonisation (ICH). The E18 guideline update, expected in 2025, will address ethnic differences in NTI drug response-a big deal for global trials. Right now, a study done in the U.S. might not be accepted in Europe or Japan without additional data. Harmonization could cut development time and cost, making NTI generics more accessible worldwide.

What’s Next? Modeling and Innovation
One of the most promising developments is the use of physiologically-based pharmacokinetic (PBPK) modeling. Instead of testing every new formulation in humans, companies can simulate how the drug behaves in different populations based on age, weight, liver function, and genetics.
The FDA ran a pilot study in 2022 using PBPK modeling for warfarin generics. Results were encouraging. The model predicted bioequivalence with high accuracy, reducing the need for large-scale clinical trials. If validated, this could become a game-changer.
But don’t expect it to replace bridging studies anytime soon. The FDA is clear: for now, clinical data remains essential. PBPK modeling might reduce the number of subjects needed or help design better studies-but it won’t eliminate them.
The Human Cost of Getting It Right
Behind every NTI generic approval is a patient. Someone managing their heart condition with digoxin. Someone on levothyroxine trying to feel normal again. Someone on phenytoin after a seizure. These drugs aren’t optional. They’re life-sustaining.
When a generic isn’t bioequivalent, the consequences aren’t theoretical. They’re real: hospitalizations, emergency visits, lost workdays, and in some cases, death. That’s why regulators can’t afford to cut corners. The cost of a mistake is measured in lives, not dollars.
But the flip side is also true. When a safe, affordable NTI generic reaches the market, it opens access to care for people who can’t afford the brand. That’s why the $32.8 billion potential market for NTI generics by 2025 isn’t just a number-it’s a promise. A promise that innovation, regulation, and patient safety can move forward together.
Final Thoughts
Bridging studies for NTI generics aren’t just a regulatory box to check. They’re a necessary safeguard. The science is complex. The stakes are high. And the path is long. But for patients who depend on these drugs, there’s no alternative to getting it right.
Manufacturers who invest in the right expertise, follow the guidelines, and prioritize patient safety aren’t just building a product-they’re building trust. And in the world of NTI drugs, trust is the most important ingredient of all.