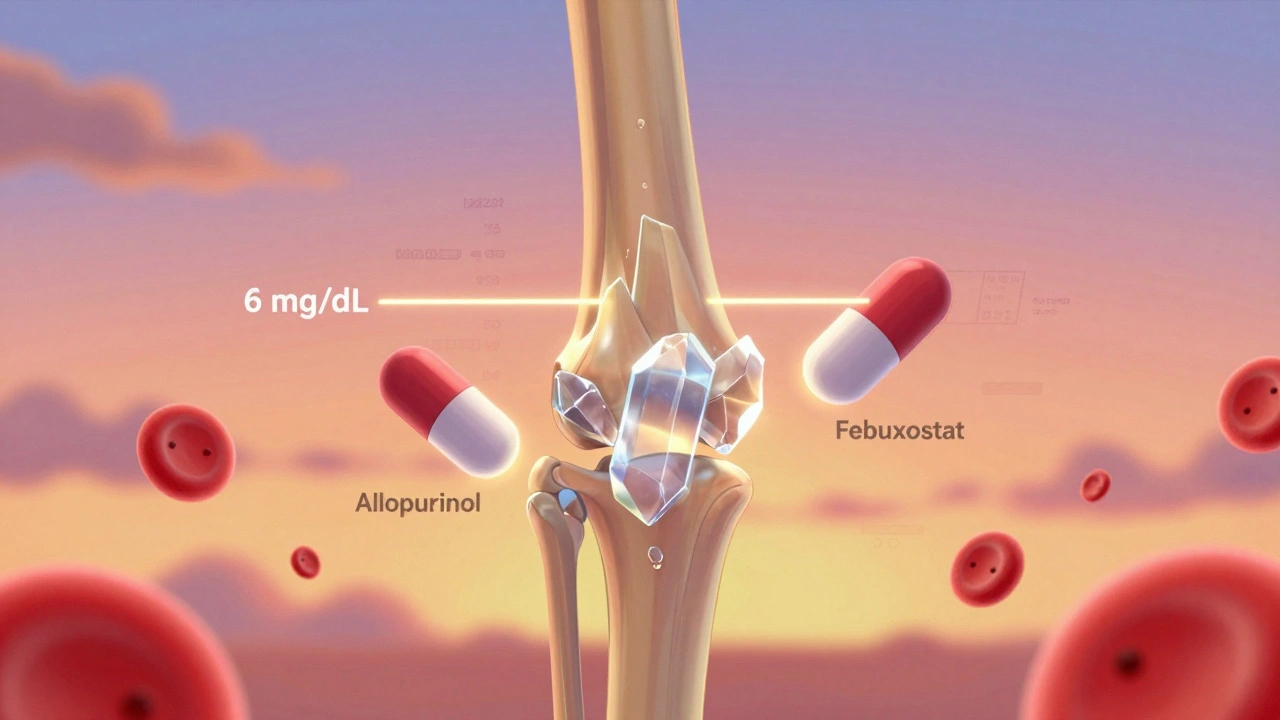
For decades, gout was seen as a painful but unavoidable condition-something you just had to live with if you ate too much red meat or drank too much beer. But that’s not true anymore. Today, we know gout is a urate targets disease. That means it’s not about managing pain alone; it’s about hitting a specific number in your blood: your serum urate level. If you can keep that number low enough, the crystals that cause the agony will slowly dissolve. And the two main drugs that make this possible are allopurinol and febuxostat.
Why 6 mg/dL Is the Magic Number
The goal isn’t to make your urate level disappear. It’s to get it below 6 mg/dL (or 360 micromol/L). That’s the saturation point-the level at which uric acid stops forming crystals in your joints. Above that, crystals form. Below it, they start to break down. This isn’t guesswork. It’s based on decades of research, including 12 randomized trials with over 3,800 patients. Studies show that keeping your urate under 6 mg/dL cuts flare frequency by 74% compared to staying above 6.8 mg/dL.
But here’s the catch: many people never get there. In New Zealand, only 42% of patients on urate-lowering therapy reach this target within a year. Why? Because most start too low and don’t adjust fast enough. Allopurinol, the first-line drug, is often started at 100 mg a day. That’s fine for mild cases. But if you’ve had multiple flares, tophi, or joint damage, you might need 400 mg, 600 mg, or even 800 mg daily. The key is not to stay stuck on a low dose. You need to titrate up-every few weeks-until your blood test shows you’ve hit the target.
Allopurinol: The Workhorse, But Not Always Enough
Allopurinol has been around since the 1960s. It’s cheap-$4 to $12 a month-and it works. But it’s not one-size-fits-all. Your kidneys handle it. If you have kidney disease, you start lower: 50 mg a day or even less. And if you’re Māori or Pacific Islander, you’re more likely to be prescribed allopurinol, but also more likely to miss your target because of barriers in care access, language, or provider bias.
Another problem: fear. Many patients stop allopurinol because they heard about a rare but serious reaction called allopurinol hypersensitivity syndrome. It’s real-but it affects only 0.1% to 0.4% of people. And the risk jumps 25 times if you carry the HLA-B*5801 gene. That’s why some places now test for it before starting, especially in high-risk groups. But in most clinics, it’s still not routine. So patients are left guessing. And that’s dangerous.
Real-world data from New Zealand shows 30% to 50% of patients need doses above 300 mg to hit their target. Some need 600 mg. Yet doctors often stop at 300 mg because they’re afraid of side effects. That’s the opposite of what guidelines say. The 2020 American College of Rheumatology guidelines say: start low, go slow, but go all the way. If you’re not at target after 2-4 months, increase the dose. Don’t give up.
Febuxostat: The Alternative When Allopurinol Fails
Febuxostat came onto the scene in the 2010s. It’s stronger, doesn’t rely on kidney function as much, and works better for people with moderate to severe kidney disease. A 2023 meta-analysis found it achieves target urate levels 15% more often than allopurinol in patients with CKD stage 3 or higher.
But it’s more expensive-$30 to $50 a month in the U.S. That’s why it’s not first-line everywhere. In New Zealand, it’s used less than allopurinol. The NICE guidelines (UK) say both drugs are equally good as first choices. The EULAR guidelines (Europe) still prefer allopurinol for people with normal kidneys. But if you’ve tried allopurinol at 600 mg for six months and your urate is still above 6 mg/dL, febuxostat is your next move.
One thing to watch: febuxostat carries a slightly higher risk of heart-related death in people with existing heart disease, according to the FDA’s 2019 warning. So if you have a history of heart attack or stroke, your doctor may avoid it. But for most people without heart disease, it’s a safe and effective option.

When You Need to Go Lower: The 5 mg/dL Target
Not everyone just needs to get under 6 mg/dL. If you have tophi-those visible lumps of urate crystals under your skin-or if you’ve had joint damage shown on X-rays, or if you’re still getting flares even at 6 mg/dL-you need to go lower. That’s where the 5 mg/dL target comes in (300 micromol/L).
The 2023 EULAR guidelines and the 2020 ACR guidelines both say: if you have severe gout, aim for under 5 mg/dL. Why? Because studies show that at this level, tophi shrink faster. One study found 89% of patients saw tophi reduce when urate stayed below 0.30 mmol/L, compared to just 72% at 0.36 mmol/L. That’s a big difference. It means fewer surgeries, less pain, and better mobility.
But here’s the catch: no one has done a randomized trial proving that 5 mg/dL is better than 6 mg/dL for long-term outcomes. The evidence is observational. That’s why some experts call it a “best guess.” Still, if you’ve got visible tophi, most rheumatologists will push you to the lower target. And if you’re on 800 mg of allopurinol or 120 mg of febuxostat and still not there, you might need to add a uricosuric drug like probenecid-or wait for new drugs like verinurad, which are in late-stage trials.
The Flare Paradox: Why Treatment Can Make Things Worse at First
One of the biggest surprises for patients is this: when you start allopurinol or febuxostat, your gout flares might get worse before they get better. That’s not a mistake. It’s normal. As crystals start to dissolve, they release particles into your joints. Your immune system sees them as invaders and triggers inflammation. It’s like stirring up a nest of hornets.
That’s why guidelines now say: always start with a low-dose anti-inflammatory when beginning urate-lowering therapy. Colchicine 0.6 mg once or twice a day for six months is the standard. Some doctors use low-dose prednisone. The point is: don’t stop the urate-lowering drug because you’re flaring. Keep going. The flares will settle in 2-3 months.
Patients who understand this are far more likely to stick with treatment. In fact, a survey of 12,450 people in the Gout Support Group on HealthUnlocked found that 62% said their biggest frustration was being told to stop their medication when they flared. That’s the wrong advice. The drug is working. You just need to protect yourself from the side effect.
Monitoring Is Non-Negotiable
You wouldn’t manage diabetes without checking your blood sugar. So why manage gout without checking your urate level? Yet in the U.S., only 54% of patients get the recommended monthly blood tests during the titration phase. In New Zealand, it’s even worse in rural areas.
Here’s the rule: test your serum urate every 2-4 weeks while you’re increasing your dose. Once you hit target, check every 6 months. If you’re not testing, you’re flying blind. You might think you’re on the right dose-but your urate could be at 7.5 mg/dL and you’d never know.
And here’s a new standard: the ACR now says you need two consecutive measurements under 6 mg/dL, at least 30 days apart, to confirm you’ve reached your target. One low number could be luck. Two in a row mean you’ve got it under control.
What About Asymptomatic High Urate?
If your urate is 8 mg/dL but you’ve never had a gout flare, should you take a drug? The answer is no. The 2020 ACR guidelines are clear: don’t treat asymptomatic hyperuricemia. There’s no proof it prevents gout, and the risks of side effects outweigh the unproven benefits. Some doctors still do it-especially if a patient is anxious-but it’s not evidence-based.
Focus on the people who need it: those with flares, tophi, or joint damage. That’s where the real impact is.
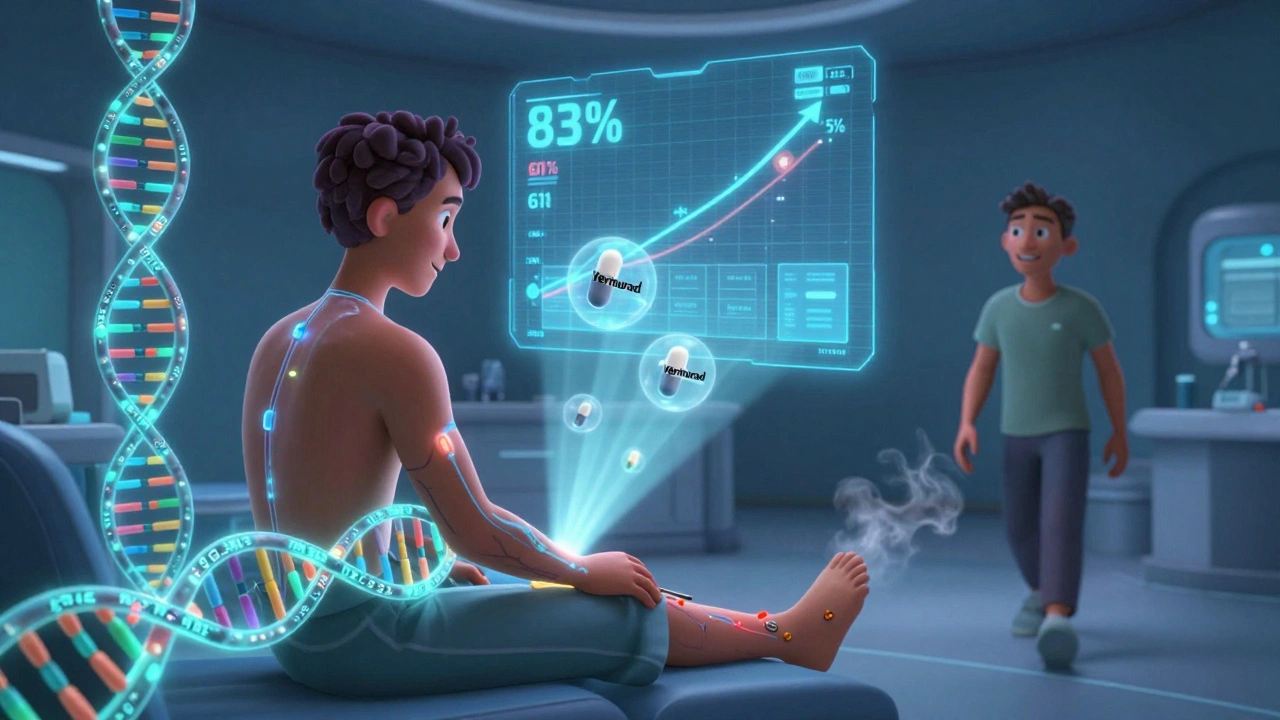
The Future: Personalized Dosing and New Drugs
One of the most exciting advances is genetic testing. A 2024 study called GOUT-PRO found that using genetic markers-like ABCG2 and SLC22A12 variants-to guide allopurinol dosing increased target achievement from 61% to 83% in just six months. That’s huge. We’re moving from guessing doses to knowing exactly how much a person needs based on their genes.
And new drugs are coming. Verinurad, a next-generation uricosuric, is in phase 3 trials. It lowers urate without needing high doses. If approved, it could help the 46% of patients who can’t reach target even on maximum allopurinol.
The ULTRA-GOUT trial, starting in 2025, will compare fixed-dose allopurinol with the traditional treat-to-target approach. We might finally know which strategy works better in the long run.
For now, the message is simple: gout is not a life sentence. It’s a biochemical imbalance. And with the right drug, the right dose, and the right monitoring, it can be controlled. Allopurinol and febuxostat aren’t magic pills. But they’re the best tools we have. Use them right, and your crystals will disappear.
What is the ideal serum urate target for most people with gout?
The standard target is below 6 mg/dL (360 micromol/L). This level prevents new urate crystals from forming and helps dissolve existing ones. Most guidelines, including those from the American College of Rheumatology and NICE, agree on this target for patients with occasional flares and no visible tophi.
When should the target be lowered to 5 mg/dL?
Lower the target to 5 mg/dL (300 micromol/L) if you have tophi, joint damage seen on X-rays, or frequent flares despite being under 6 mg/dL. This stricter target helps dissolve crystals faster and reduces tophus size. Evidence shows up to 89% of patients see tophi shrink at this level, compared to 72% at 6 mg/dL.
Is allopurinol safe at high doses like 600 mg or 800 mg daily?
Yes, allopurinol is safe at doses up to 800 mg daily in people with normal kidney function. The risk of serious side effects like hypersensitivity syndrome is very low-only 0.1% to 0.4%-and even lower if you don’t carry the HLA-B*5801 gene. Most patients who don’t reach their target aren’t taking enough, not too much.
Why do gout flares get worse when I start taking allopurinol or febuxostat?
As urate crystals dissolve, they release particles into your joints, triggering inflammation. This is called the "flare paradox." It doesn’t mean the drug isn’t working-it means it is. Taking a low daily dose of colchicine (0.6 mg) for 6 months while starting urate-lowering therapy prevents most of these flares.
Do I need to take urate-lowering drugs forever?
Yes, for most people. Gout is a chronic condition caused by long-term urate buildup. Stopping the drug will let urate levels rise again, and crystals will reform. You don’t need to take it for life if you’ve fully dissolved all crystals and stayed under 5 mg/dL for 2+ years-but that’s rare. Most people need ongoing treatment to stay symptom-free.
Can I switch from allopurinol to febuxostat if I’m not reaching my target?
Yes, if you’re on maximum allopurinol (600-800 mg/day) for at least 3 months and your urate is still above target, switching to febuxostat is a standard next step. Febuxostat is more effective in people with kidney disease and often achieves target levels faster. Your doctor will monitor for heart-related risks, especially if you have a history of heart disease.
How often should I get my serum urate tested?
Test every 2-4 weeks while adjusting your dose. Once you reach your target, test every 6 months. Monthly testing during titration increases your chance of hitting target by 31%. Don’t skip tests-even if you feel fine. Your symptoms don’t tell you your urate level.
Is febuxostat better than allopurinol?
It depends. For people with normal kidney function, allopurinol is just as effective and much cheaper. For those with moderate to severe kidney disease, febuxostat works better and is safer. If you’ve tried allopurinol at high doses and still haven’t reached target, febuxostat is your best next option.
Should I get tested for the HLA-B*5801 gene before starting allopurinol?
It’s strongly recommended if you’re of Asian, African, or Māori/Pacific Islander descent, as these groups have higher rates of the gene. Even if you’re not, if you’ve had a previous reaction to allopurinol, testing is wise. It’s a simple blood test that can prevent a rare but life-threatening reaction.
What if I can’t reach my urate target even on high-dose allopurinol or febuxostat?
You’re not alone-about 46% of patients struggle with this. Options include adding a uricosuric like probenecid, switching to a combination therapy, or waiting for newer drugs like verinurad, which are in late-stage trials. In severe cases, pegloticase (an IV drug) may be used. Talk to a rheumatologist. There are still options.

12 Comments
Deborah Jacobs
I’ve been on allopurinol for 3 years now, and honestly? It saved my life. Used to be bedridden for weeks after a flare. Now I hike, dance, even cook spicy food again. The key? Not giving up when the first few months sucked. My doc upped my dose to 600mg after 4 months - and boom, no more flares. I cried the first time I woke up without pain. It’s not magic, it’s math. And math works.
Also, colchicine during titration? Non-negotiable. I took it like vitamins. No drama. No panic. Just calm, steady progress. If you’re scared of side effects - talk to your rheum. Don’t quit.
Also also - get your urate tested. Like, actually. Not just when you feel like it. Your body doesn’t lie. Your pain? That’s just the alarm. The real signal’s in the blood.
And yes, I’m still on it. Forever? Probably. But I’d rather be alive and on meds than dead and ‘natural’.
Lucy Kavanagh
Have you ever wondered why the NHS only tests urate levels every 6 months? Because Big Pharma doesn’t want you to know how easy it is to fix gout. They make billions off painkillers and fancy infusions. Allopurinol costs less than a latte. Why isn’t it in every GP’s drawer? Why do we need genetic tests? Why are we being gaslit into thinking this is ‘complicated’? It’s not. It’s control. They want you dependent. I stopped all meds after 2 years and went vegan. Flares? Gone. Coincidence? I think not.
Also - febuxostat? That’s the drug they push when allopurinol fails. But what if allopurinol never should’ve been your first choice? What if the whole ‘titrate up’ thing is just a scam to keep you on pills longer? I say: low urate = no crystals. No crystals = no gout. Why not just eat less meat and drink water? Simple. But boring. So they sell you a pill.
Question: who profits if you’re cured? Exactly.
Stephanie Fiero
okay so i just got diagnosed last month and i was like ‘wait so i dont have to just suffer forever???’ and then i read this and i cried. like actual tears. i thought gout was my punishment for loving beer and steak. turns out it’s just chemistry. and i can fix it. i’m on 300mg allopurinol now and my doc says we’ll bump it up in 6 weeks. i’m scared but also… hopeful? like, i can actually be normal again? i don’t want to be ‘that guy’ who can’t go to BBQs. i want to live. thanks for writing this. i’m not alone.
ps: i’m taking colchicine like a good girl. no flares yet. fingers crossed. 💪
Jennifer Patrician
ALLOPURINOL IS A LIE. The FDA knew about HLA-B*5801 since 2008. They buried it. Why? Because if they tested everyone, they’d have to recall every generic bottle. And then who’d buy the $50 febuxostat? You think your doctor cares about you? Nah. They get paid per visit, not per cure. They don’t want you cured. They want you coming back every month with a new flare. That’s the business model. And now they’re pushing genetic testing like it’s a miracle? It’s just a new revenue stream. Wake up. The crystals aren’t the enemy. The system is.
Also - ‘titrate up’? That’s just code for ‘we’re not sure how much to give you so we’ll guess for 6 months.’ You’re a guinea pig. And I’m not taking it.
Ali Bradshaw
Been there. Done that. Took me 18 months to get my urate under 6. My doc kept saying ‘you’re doing great’ while my levels were at 7.2. I finally demanded a copy of my labs. Saw the pattern. Went back with a printed chart. He apologized. Changed my dose. Hit target in 6 weeks.
Point is: you have to be your own advocate. No one else is going to fight for you. Don’t wait for permission. Ask for the numbers. Push for the dose. Your body’s worth it.
Also - colchicine during titration? Do it. Even if you feel fine. Prevention > reaction.
And yeah, it’s lifelong. But so is brushing your teeth. You don’t stop brushing because your teeth feel fine. You do it because you know what happens if you don’t.
Annie Grajewski
So let me get this straight - we’re supposed to believe that a $4 pill that’s been around since Nixon’s presidency is the gold standard… but only if you’re white, rich, and have a rheumatologist who actually reads guidelines? Meanwhile, my cousin in Alabama got prescribed 100mg for 2 years and was told ‘it’s just gout, drink more water.’ He lost three toes. But hey - at least he didn’t need a genetic test, right? The system is a joke. We treat gout like it’s a moral failing. It’s not. It’s a biochemical glitch. And we’ve got the tools. We just don’t care enough to use them right.
Also - ‘asymptomatic hyperuricemia’? That’s just a fancy way of saying ‘you’re not sick yet, so we’ll ignore you until you are.’ Classic medicine. Let the pain do the talking. Then they’ll act. Pathetic.
Mark Ziegenbein
The entire paradigm of gout management is predicated on a flawed assumption: that urate is the sole causal agent. But what if it’s not? What if urate is merely a biomarker - a symptom of systemic inflammation, oxidative stress, mitochondrial dysfunction, and gut dysbiosis? The pharmaceutical industry has commodified reductionism. They sell you a pill that lowers serum urate, but they never ask why your liver is overproducing it. Why your kidneys are underexcreting it. Why your microbiome is screaming for fiber. You’re not treating the disease. You’re treating a shadow on the wall. The real cure lies in epigenetics, circadian rhythm optimization, and polyphenol-rich diets - not in a pill you swallow while scrolling Instagram. Allopurinol is a Band-Aid on a hemorrhage. And febuxostat? A more expensive Band-Aid. We’ve lost the forest for the trees. And we call this medicine.
Also - ‘titrate up’? That’s not medicine. That’s trial and error with a clipboard.
Rupa DasGupta
OMG I’m so glad someone finally said this 😭 I’ve been on allopurinol for 5 years and my doc never told me about the 5 mg/dL target until I cried in his office last year. I had tophi on my elbow. Like, visible. People stared. I wore long sleeves in summer. I was so ashamed. Then he said ‘try 5.’ I cried again. And guess what? In 8 months? Gone. Just… gone. Like magic. I still take meds. I still test. I still feel like I’m fighting a war. But now I know I’m winning. Thank you for writing this. I feel seen. 💛
Marvin Gordon
One thing no one talks about: the mental toll. You think gout is just pain? Nah. It’s shame. It’s being the guy who can’t drink beer at the office party. It’s avoiding family BBQs because you’re scared you’ll ‘mess up.’ It’s the guilt when you ‘fail’ and flare again. I didn’t know that until I started taking colchicine daily and actually felt… normal. Like, I could breathe. I could plan a weekend. I could sleep through the night. This isn’t just about numbers. It’s about reclaiming your life. And yeah - it takes time. But you’re not broken. You’re just unmanaged. Fix the dose. Fix the monitoring. Fix your mindset. You got this.
ashlie perry
they’re lying about febuxostat and heart risks. i know a guy who took it for 3 years and his heart is better than his 25-year-old son’s. they just want you scared so you’ll stick with allopurinol. and allopurinol is a scam. why do you think it’s so cheap? because it’s old. and old drugs don’t make money. so they make up scary stories. i’m switching. and i’m not sorry.
Juliet Morgan
just wanted to say - if you’re reading this and you’re scared to ask your doctor for a higher dose? do it. i was too. i thought i’d be ‘that patient.’ turns out, my doc was relieved. said 80% of patients don’t get to target because they’re afraid to push. you’re not being annoying. you’re being smart. i’m on 600mg now. no flares in 11 months. i’m alive. thank you for this post. it gave me courage.
Norene Fulwiler
As a Māori woman who’s been through this - I want to say: the system fails us. We get the same meds, but not the same care. My cousin got 100mg for 3 years. No tests. No questions. Just ‘take this.’ Meanwhile, her white coworker got genetic testing and a 600mg dose in 3 months. It’s not about the drug. It’s about who you are. I had to go to a private clinic to get the care I needed. And I’m lucky I could afford it. This isn’t just medicine. It’s justice. We need to fix that.
Also - I tested positive for HLA-B*5801. They didn’t tell me before I started allopurinol. That’s not just negligence. That’s violence.